Methods for Draping Surgical Incision Sites
Folder:
Year:
Abstract:
Disclosed are methods for draping a surgical incision site prior to surgery. Specifically, the methods of this invention involve the in situ formation of a cyanoacrylate polymeric drape over the skin surface at the surgical incision site. An incision is then made through this surface and the surgery is then conducted through the incision
Type of document:
Language:
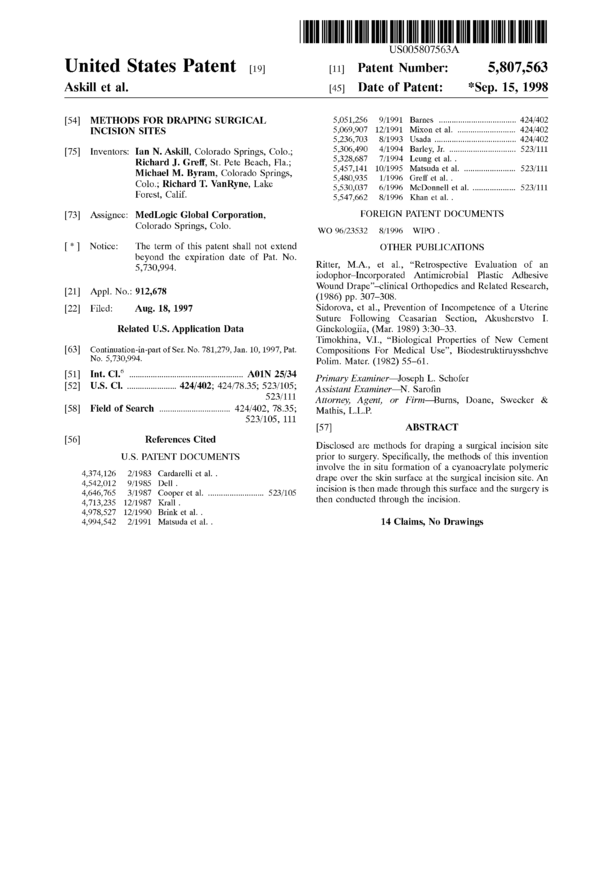
US005807563A
Ulllted States Patent [19] [11] Patent Number: 5,807,563
Askill et al. [45] Date of Patent: *Sep. 15, 1998
[54] METHODS FOR DRAPING SURGICAL 5,051,256 9/1991 Barnes .................................. .. 424/402
INCISION SITES 5,069,907 12/1991 Mixon et al. 424/402
5,236,703 8/1993 Usada . . . . . . . . . . . . . .. 424/402
[75] Inventors: [an N_ Askill, Colorado Springs, Colo‘; 5,306,490 4/1994 Barley, Jr. ............................. .. 523/111
Richard J. Grefi', St. Pete Beach, Fla.; 17/199;‘ Leungdet ‘*1~~1
Michael M_ Byram’ Colorado Springs’ , , 0/199 Matsu a eta. ...................... .. 523/111
C 1 . R, h d T V R k 5,480,935 1/1996 Greff et al. .
0 °~> 1° F“ - 3“ V119» La 6 5,530,037 6/1996 McDonnell et al. .................. .. 523/111
FOFCSE Cahf 5,547,662 8/1996 Khan etal..
[73] Assignee: MedLogic Global Corporation, FOREIGN PATENT DOCUMENTS
Colorado Springs’ Colo" WO 96/23532 8/1996 WIPO .
[ * ] Notice: The term of this patent shall not extend OTHER PUBLICATIONS
beyond the expiration date of Pat. No. . .
5,730,994. Ritter, M.A., et al., “Retrospective Evaluation of an
iodophor—Incorporated Antimicrobial Plastic Adhesive
. Wound Drape”—clinical Orthopedics and Related Research,
[21] Appl. No.. 912,678 (1986) pp. 307_308.
[22] Filed: Aug. 18, 1997 Sidorova, et al., Prevention of Incompetence of a Uterine
Suture Following Ceasarian Section, Akusherstvo I.
Related U.S. Application Data Ginekologiia, (Mar. 1989) 3:30-33.
Timokhina, V.I., “Biological Properties of New Cement
[63] Continuati0n—in—part of Ser. No. 781,279, Jan. 10, 1997, Pat. Compositions For Medical Use”, Biodestriiktiruysshchve
N°~ 5»730»994~ Polim. Mater. (1982) 55-61.
[51] Int. Cl.o .. .......................... .. A01N 25/34 Primary Exammer_JoSeph L. Schofer
[52] U.S. Cl. ..................... .. 424/402; 424/78.35; 523/105; Assistant Exammer_N. Sarofin
523/111 Attorney, Agent, or Firm—Burns, Doane, Swecker &
[58] Field of Search ............................... .. 424/402, 78.35; Mathis, LL13.
523/105, 111
[57] ABSTRACT
56 R f C't d . . . . . . .
[ ] e erences 1 e Disclosed are methods for draping a surgical incision site
U.S. PATENT DOCUMENTS prior to surgery. Specifically, the methods of this invention
4,374,126 2/1983 Cardarem et al. . involve the in sitii formation of a cyanoacrylate polymeric
drape over the skin surface at the surgical incision site. An
4,542,012 9/1985 Dell . . . . . . .
4,646,765 3/1987 Cooper et al. ........................ .. 523/105 “@510” 15 then made thmugh ‘h.1S.5“rfa"‘°* and the Surgery 15
4,713,235 12/1987 Km“ . then conducted through the incision.
4,978,527 12/1990 Brink et al. .
4,994,542 2/1991 Matsuda et al. . 14 Claims, No Drawings
5,807,563
1
METHODS FOR DRAPING SURGICAL
INCISION SITES
CROSS-REFERENCE TO RELATED
APPLICATIONS
This application is a continuation-in-part of application
Ser. No. 08/781,279 filed on Jan. 10, 1997 now U.S. Pat. No.
5,730,994 which application is incorporated herein by ref-
erence in its entirety.
BACKGROUND OF THE INVENTION
1. Field of the Invention
This invention is directed to methods for draping a
surgical incision site prior to surgery. Specifically, the meth-
ods of this invention involve the in situ formation of a
polymeric cyanoacrylate drape over a mammalian skin
surface at the surgical incision site. An incision is made
through the drape and surgery is then conducted through the
incision.
2. References
The following publications, patent applications and pat-
ents are cited in this application as superscript numbers:
1 Masterson, M. D., “Skin Preparation”, Chapter 9, in
Surgical Infections, Diagnosis and Treatment, Meakins, Ed.,
Scientific American, Inc., New York, USA, Publisher, pp.
119-125 (1994)
2 Osuna, et al., “Comparison of anAntimicrobialAdhesive
Drape and Povidone-Iodine Preoperative Skin Preparation
in Dogs”, Veterinary Surgery, 21(6):458—462 (1992)
3 Hagen, et al., “A Comparison of Two Skin Preps Used in
Cardiac Surgical Procedures”, AORN Journal, 62(3)
:393-402 (1995)
4 Alexander, et al., “Development of a Safe and Ejfective
One-Minute Preoperative Skin Preparation”, Arch. Surg.,
120:1357-1361 (1985)
5 Chiu, et al., “Plastic Adhesive Drapes and Wound
Infection After Hip Fracture Surgery”, Aust. N. Z. J. Surg.,
63:798-801 (1993)
6 Barley, “Methods for Retarding Blister Formation by
Use of Cyanoacrylate Adhesives”, U.S. Pat. No. 5,306,490,
issued Apr. 26, 1994.
7 Barley, et al., Methods for Treating Suturable Wounds
by Use of Sutures and Cyanoacrylate Adhesives, U.S. Pat.
No. 5,254,132, issued Oct. 19, 1993
8 McIntire, et al., Process for the Preparation of Poly(ot-
Cyanoacrylates), U.S. Pat. No. 3,654,239, issued Apr. 4,
1972
9 Barley, et al., International Patent Application Publica-
tion No. WO 93/25196, for Methods for Treating Non-
Suturable Wounds by Use of Cyanoacrylate Adhesives,
published Dec. 23, 1993
10 Barley, et al., Methods for Reducing Skin Irritation
From Artificial Devices by Use of Cyanoacrylate Adhesives,
U.S. Pat. No. 5,653,769, issued Aug. 5, 1997
11 Tighe, et al., Methods for Inhibiting Skin Ulceration by
Use of Cyanoacrylate Adhesives, U.S. Pat. No. 5,403,591,
issued Apr. 4, 1995
12 Tighe, et al., for Use of Cyanoacrylates for Providing
a Protective Barrier, U.S. Pat. No. 5,580,565, issued Dec. 6,
1996.
13 Ritter, et al., “Retrospective Evaluation of an lodophor-
Incorporated Antimicrobial Plastic Adhesive Wound
Drape”, Clinical Orthopedics and Related Research, pp.
307-308 (1988)
10
15
20
25
30
35
40
45
50
55
60
65
2
14 Duhaime, et al., “Distribution of Bacteria in the Oper-
ating Room Environment and its Relation to Ventricular
Shunt Infections: a Prospective Study”, Child’s Nerv. Syst.,
7:211-214 (1991)
15 O’Sullivan, et al., High Viscosity Cyanoacrylate Adhe-
sive Compositions, and Process for Their Preparation, U.S.
Pat. No. 4,038,345, issued Jul. 26, 1977
All of the above publications, patent applications and
patents are herein incorporated by reference in their entirety
to the same extent as if each individual publication, patent
application or patent was specifically and individually indi-
cated to be incorporated by reference in its entirety.
3. State of the Art
Reduced morbidity and/or infection associated with sur-
gical procedures necessitates the thorough preparation of the
patient’s skin prior to initiating any incision into the skin as
part of the surgical procedure. The primary reason for patient
skin preparation is to reduce the risk of wound infection by
introduction of microbes into the incision sitel from either
endogenous sources or from air borne microbes.” In turn,
reduction in such risk correlates, obviously, with reductions
in the population of microbes on the skin surface and
especially at the skin surface adjacent to the incision site.
Suitable skin preparation involves, for example, applica-
tion of an antimicrobial agent onto and around the skin
surface adjacent to the incision site which reduces the
population of microbes on these surfaces and, hence the
relative risk of infection. However, the skin is never com-
pletely sterilized during these procedures and microbes from
hair follicles and sweat/sebaceous glands will migrate to the
surface of the skin thereby raising microbial populations and
accordingly relative infection risks.2 To counter possible
microbial migration into the incision, it has become com-
mon practice to employ a surgical incise drape over the
patient’s incision site.
Conventional surgical incise drapes include those which
comprise preformed, sized polymeric films coated with a
pressure-sensitive adhesive. In some cases, an antimicrobial
agent is incorporated directly into the adhesive in order to
permit a continuous release of the antimicrobial agent onto
the skin.3’13 After application of an antimicrobial agent onto
the skin surface of the patient, the surgical incise drape is
applied, adhesive side down, with pressure to effect adher-
ence of the drape to the skin. Asurgical incision is then made
through the drape and the requisite surgery is conducted
through this incision. After completion of the surgery, the
drape is conventionally removed from the skin surface.
Notwithstanding the benefits associated with a surgical
incise drape, several problems exist which have both limited
the general applicability of these drapes to surgical incisions
and have actually increased the relative risk of infection.
Specifically, the first most common and potentially serious
problem associated with the use of conventional surgical
incise drapes is the separation or lifting of the drape from the
skin surface during surgery. In one study, it was reported that
up to 44% of the drapes experienced at least partial sepa-
ration during human surgery2. In turn, Alexander, et al.4
report a sixfold increase in infection rates in operations in
which the surgical incise drape separated from the skin
during surgery as compared to infection rates in which the
drape did not separate from the skin. Without being limited
by any theory, it is generally believed that occlusion of the
skin by the surgical incise drape provides a moist, warm skin
surface which can encourage microbial growth. It is further
believed that separation of the drape from the skin during
surgery permits migration of microbes and/or microbial
5,807,563
3
growth at these sites and, accordingly, in such cases, the use
of a drape can actually promote rather than retard microbial
populations at the incision site.
Non-adherence of the surgical incise drape to the patient’s
skin is, of course, related to adhesive failure as well as
wrinkling of the preformed polymeric film during applica-
tion. In the former case, this has lead to some attempts to
increase the amount and/or strength of adhesive employed in
the drape to secure the drape to the mammalian surface.
However, this in turn may lead to more rather than fewer
complications. In particular, since the drape is convention-
ally removed from the skin after surgery by, e.g., the peeling
or pulling off of the drape, an increase in the relative strength
of the adhesive leads to increased difficulty in so removing
the drape from the skin. The effort required to effect such
removal can lead to skin tearing, especially adjacent to the
incision site, as well as removal of surface hair. Skin tearing
is clearly disadvantageous and invariably raises additional
infection risks because the mammmalian skin surface is
opened (compromised) and susceptible to infection.
Moreover, the removal of hair (shaving) has also been
associated with increased infection rates2 and hair removal
due to adhesive/drape removal from the mammalian skin
can also be expected to provided similar increased infection
rates.
In the latter case, wrinkling of the polymeric drape is
essentially irreversible because the wrinkles cannot be
smoothed out absent complete removal of the drape and
drapes, once removed, cannot typically be reapplied.
Additionally, air pockets found in the wrinkles of such
drapes are undesirable because they provide a source of
microbes adjacent to the skin and, in some cases, promote
microbial growth. Wrinkling of the polymeric film is com-
mon to most applications of the surgical incise drapes but is
particularly problematic with contoured surfaces such as
elbows, knees, bony hips, etc. This, in turn, potentially limits
the use of such conventional drapes.
An additional problem associated with preformed poly-
meric films used as surgical incise drapes arises because
such drapes do not conform well to the three dimensional
contours of the human or other mammalian body thereby
increasing the possibility of separation during surgery. For
example, while abdominal area through which the surgical
incision is made is typically a good candidate for such
conventional surgical incise drapes, other surfaces such as
elbow, knee, foot, and bony hip surfaces (as examples) have
three dimensional contours which render consistent adher-
ence of the drape over the incision site during surgery
problematic at best. In this regard, Chiu, et al.5 report that
the use of sterile adhesive drapes during hip fracture sur-
geries appeared to have actually encouraged microbial accu-
mulation in the skin adjacent to the wound.
Still a further problem arises from the fact that many
adhesives employed with the polymeric films do not adhere
well to hair thereby limiting their utility2. Additionally, as
noted above, shaving to remove hair prior to surgery has
been clinically associated with increased wound infection
rates.1
In an alternative embodiment, the art has proposed the use
of emulsions/solutions containing a volatile organic solvent
and a polymer. Upon application to the skin, the solvent
dissipates leaving a polymeric film which acts as the incise
drape. Significant problems exist with such a procedure and,
in particular, the polymeric film lacks strong adhesion to the
skin and the volatile solvent can create irritation (e.g., skin,
nose, etc.) as well as can be the source of a fire hazard in the
operating room.
10
15
20
25
30
35
40
45
50
55
60
65
4
Lastly, while the most important purpose of using surgical
incise drapes is to prevent postoperative wound infections,
the simple fact of the matter is that the drapes of prior art are
removed after surgery and there is, accordingly, no postop-
erative antimicrobial effect available to the skin surface at
the surgical incision site.
This invention is directed, in part, to the discovery that the
in situ formation of a cyanoacrylate polymeric drape at the
surgical incision site prior to surgery overcomes many of the
prior art problems associated with the use of conventional
preformed surgical incise drapes and additionally provides
incremental advantages heretofore not achieved by conven-
tional drapes. For example, the cyanoacrylate polymer is
known in the art to have bacteriostatic properties and the
cyanoacrylate monomer permits the inclusion of compatible
antimicrobial agents if such is desired. Still another advan-
tage is the formation of an appropriately configured drape
without the need to modify the dimensions provided with
commercial polymeric drapes. Still further, the methods of
this invention result in incise drapes which mold directly to
the multiple contours of the intended surgical site.
The use of cyanoacrylate polymers per this invention is in
contrast to their known medical uses as an alternative or
adjunct to sutures7 or as a hemostat8. Other described uses
of cyanoacrylate prepolymers include their use to prevent
friction blister formations, treating small non-suturable
woundsg, and in inhibiting surface skin irritation arising
from friction between the skin surface and artificial devices
such as tapes, prosthetic devices, casts, and the like.”
SUMMARY OF THE INVENTION
This invention is directed to methods for draping a
surgical incision site by application of a cyanoacrylate
composition to the surface of the surgical incision site.
In situ polymerization of the cyanoacrylate composition
provides for an adherent polymeric film over the surgical
incision site which acts as a surgical incise drape during
surgery. The adherence of the polymeric film to the skin
surface is so strong that the possibility of separation of the
drape during surgery is effectively removed. Additionally,
the cyanoacrylate composition can be applied as a liquid/gel
to the skin surface which permits formation of an adherent
film over any skin contour including elbows, knees, hips,
and the like.
Since the polymeric film is naturally shed from the skin
surface 1-4 days after application, there is no need to effect
removal of the drape after surgery or to cause the skin
trauma potentially associated with drape removal. This
polymeric film forms a bacteriostatic or bactericidal barrier
to external sources of wound contamination. Moreover, in a
preferred embodiment, the cyanoacrylate composition is
formulated to contain an antimicrobial agent which, over
time, will be released from the resulting film thereby pro-
viding for peri- and post-surgical infection protection not
now available from conventional drapes.
Accordingly, in one of its method aspects, this invention
is directed to a method for forming an adherent, surface
conforming drape at a surgical incision site of a patient
which method comprises:
(a) defining a surgical incision site on the patient;
(b) applying a sufficient amount of a composition com-
prising a polymerizable cyanoacrylate ester to the skin
surface at the surgical incision site defined in (a) above
so as to cover this site with the composition;
(c) polymerizing the cyanoacrylate ester so as to form a
flexible, waterproof, adhesive polymer layer which
5,807,563
5
adheres to the area(s) where the composition was
applied and which layer has a thickness of from about
2 to about 500 microns; and
(d) creating an incision through the polymer layer formed
in (c) above.
Application of the layer of composition comprising the
cyanoacrylate ester is preferably made onto the surface of
intact or injured skin and the incision is made subsequent to
formation of the cyanoacrylate polymer layer. More
preferably, the skin is intact skin further characterized as
lacking any infection, open wounds, etc. which would
permit the polymer to penetrate from the surface of the
epidermis to or beyond the dermal layer.
Preferably, the polymerizable cyanoacrylate ester com-
prises an ester which, in monomeric form, is represented by
formula I:
0 1
II
CH2 =(|I — COR
CN
where R is selected from the group consisting of:
alkyl of 1 to 10 carbon atoms,
alkenyl of 2 to 10 carbon atoms,
cycloalkyl groups of from 5 to 8 carbon atoms,
phenyl,
2-ethoxyethyl,
3-methoxybutyl,
and a substituent of the formula:
R’ o
I ll
—(|Z—COR"
R,
wherein each R‘ is independently selected from the group
consisting of:
hydrogen and methyl, and
R“ is selected from the group consisting of:
alkyl of from 1 to 6 carbon atoms,
alkenyl of from 2 to 6 carbon atoms,
alkynyl of from 2 to 6 carbon atoms,
cycloalkyl of from 3 to 8 carbon atoms,
aralkyl selected from the group consisting of benzyl,
methylbenzyl and phenylethyl,
phenyl, and
phenyl substituted with 1 to 3 substituents selected from
the group consisting of hydroxy, chloro, bromo, nitro,
alkyl of 1 to 4 carbon atoms, and alkoxy of from 1 to
4 carbon atoms.
More preferably, in the cyanoacrylate esters of formula I,
R is alkyl of from 2 to 10 carbon atoms and more preferably
alkyl of from 2 to 8 carbon atoms. Even more preferably, R
is butyl, pentyl or octyl and most preferably, R is n-butyl.
In another preferred embodiment, the polymerized
cyanoacrylate composition has a thickness of no more than
about 1 millimeter and, more preferably, the polymer layer
has a thickness of from about 2 to about 500 microns and
still more preferably from about 20 to about 100 microns.
DETAILED DESCRIPTION OF THE
PREFERRED EMBODIMENTS
This invention is directed to methods for draping a
surgical incision site prior to surgery. However, prior to
10
15
20
25
30
35
40
45
50
55
60
65
6
discussing this invention in further detail, the following
terms will first be defined.
Definitions
As used herein, the following terms have the following
meanings:
The term “surgical incision site” refers to the skin surface
to which the surgical incision is to be made as well as the
immediate area adjacent to the incision. This immediate area
typically extends at least 0.1 to 2 inches (0.254 to 5.08 cm)
in all directions beyond the incision and preferably extends
by about 0.25 to 12 inches (0.635 cm to 30.48 cm) beyond
the incision.
The term “incision” or “surgical incision” refers to any
surgical penetration which extends beyond the dermal or
epidermal layer of the patient’s skin and includes, by way of
example, incisions or punctures made by needles, knives
(including surgical knives, surgical cautery knives, and the
like), lasers (medical surgical laser), trocars, IV punctures,
blood transfusion/donation punctures, vaccine inoculation
punctures, medicament punctures (e.g., insulin injections),
punctures associated with hemodialysis, etc.
The term “polymerizable cyanoacrylate esters” refers to
polymerizable formulations comprising cyanoacrylate
monomers or polymerizable oligomers which, in their
monomeric form, are preferably compounds represented by
formula I as described above.
More preferably, in formula I, R is an alkyl group of from
2 to 10 carbon atoms including ethyl, n-propyl, iso-propyl,
n-butyl, isobutyl, sec-butyl, n-pentyl, iso-pentyl, n-hexyl,
iso-hexyl, 2-ethylhexyl, n-heptyl, octyl, nonyl, and decyl.
More preferably, R is butyl, pentyl or octyl and most
preferably, R is n-butyl. Mixtures of such compounds can
also be employed.
Apreferred cyanoacrylate ester for use in the invention is
n-butyl-2-cyanoacrylate.
The polymerizable cyanoacrylate esters described herein
rapidly polymerize in the presence of water vapor or tissue
protein, and the n-butyl-cyanoacrylate bonds to mammalian
skin tissue without causing histotoxicity or cytotoxicity.
Such polymerizable cyanoacrylate esters are sometimes
referred to herein as prepolymers and compositions com-
prising such esters are sometimes referred to herein as
prepolymer compositions.
Polymerizable cyanoacrylate esters are known in the art
and are described in, for example, U.S. Pat. Nos. 3,527,224;
3,591,676; 3,667,472; 3,995,641; 4,035,334; and 4,650,826
the disclosures of each are incorporated herein by reference
in their entirety.
The term “biocompatible plasticizer” refers to any mate-
rial which is soluble or dispersible in the cyanoacrylate
composition, which increases the flexibility of the resulting
polymeric film coating on the skin surface, and which, in the
amounts employed, is compatible with the skin as measured
by the lack of moderate to severe skin irritation. Suitable
plasticizers are well known in the art and include those
disclosed in U.S. Pat. Nos. 2,784,127 and 4,444,933 the
disclosures of both of which are incorporated herein by
reference in their entirety. Specific plasticizers include, by
way of example only, acetyl tri-n-butyl citrate (preferably
~20 weight percent or less), acetyl trihexyl citrate
(preferably ~20 weight percent or less) butyl benzyl
phthalate, dibutyl phthalate, dioctylphthalate, n-butyryl tri-
n-hexyl citrate, diethylene glycol dibenzoate (preferably ~20
weight percent or less) and the like. The particular biocom-
5,807,563
7
patible plasticizer employed is not critical and preferred
plasticizers include dioctylphthalate and C2-C4-acyl tri-n-
hexyl citrates.
The term “surgical incision drape” refers to the drape
formed over the surgical incision site and through which the
surgical incision is made. The term surgical incision drape is
synonymous with the term “incise drape” as used by Osuna,
et al.2
The term “antimicrobial agent” refers to agents which
destroy microbes (i.e., bacteria, fungi, yeasts and viruses)
thereby preventing their development and their pathogenic
action.
Methods
The methods of this invention comprise the in situ for-
mation of a cyanoacrylate polymer film on the skin surface
at the surgical incision site of a patient which polymeric film
acts as a surgical incision drape.
The surgical protocol preferably involves skin preparation
prior to in situ formation of the cyanoacrylate polymer drape
over the surgical incision site. Specifically, an antimicrobial
agent is applied to the cleaned surgical incision site. The
antimicrobial agent can be any suitable agent including
iodine based solutions, alcohols, etc. In one embodiment, an
iodine prep solution is first applied to the surgical incision
site. The patient’s skin is then cleansed and scrubbed with
this solution and subsequently washed off. Afterwards, an
alcohol solution or a povidone iodine solution is applied to
the surgical incision site to complete the skin preparation.
The surgical incision site is preferably dried and then an
adherent polymeric drape is formed over this site by apply-
ing a cyanoacrylate adhesive composition to the skin surface
at the surgical incision site. As noted above, this composition
comprises polymerizable cyanoacrylate monomers and/or
reactive oligomers which, upon contact with the surface skin
moisture, tissue protein, etc. polymerizes in situ to form a
polymeric film.
Polymerization occurs at ambient skin temperature while
maintaining the skin surface under suitable conditions to
allow polymerization to proceed. In general, the particular
length of time required for polymerization will vary depend-
ing on factors such as the amount of adhesive composition
applied, the temperature of the skin, the moisture content of
the skin, the surface area of skin to which the adhesive was
applied, and the like. However, in a preferred embodiment,
polymerization is generally complete within about 10 to
about 60 seconds while the skin is maintained at ambient
conditions; however, in some cases, polymerization can
occur up to about 5 minutes. During this period, the patient
is maintained in a position which permits the cyanoacrylate
to polymerize and form a polymeric drape while minimizing
any patient movement which might dislodge the cyanoacry-
late from that surgical incision site or create undesirable
bonding.
Sufficient amounts of the composition are employed to
cover (i.e., coat) the entire surgical incision site with a layer
of the cyanoacrylate polymer. If necessary, excess
cyanoacrylate monomer and/or oligomer can be removed
from the skin with a wipe or tissue paper before polymer-
ization or, after polymerization, any polymer formed at
unintended sites can be removed with materials such as
acetone (nail polish remover).
After polymerization, the resulting polymeric film forms
a surgical incise drape which strongly adheres to the skin, is
flexible and waterproof. Such strong adherence effectively
eliminates the possibility that the drape will separate from
10
15
20
25
30
35
40
45
50
55
60
65
8
the patient’s skin during surgery. However, notwithstanding
such strong adherence, the polymeric film defining the drape
will only adhere to the skin for a period of about 1-4 days
after which time it sloughs off. This occurs because the
cyanoacrylate polymer adheres only to the uppermost por-
tion of the epidermal layer which is continuously in the
process of being sloughed off and replaced by the underlying
cells. Accordingly, the cyanoacrylate drape need not be
removed in the manner of conventional preformed drapes
attached through an adhesive layer whose removal can result
in skin trauma.
The polymeric drape should be maintained in an unbroken
manner over the entire surgical incision site. This can be
assured by careful application of the cyanoacrylate adhesive
onto the skin. Additionally, the use of a plasticizer will
facilitate the maintenance of the polymeric drape in an
unbroken manner and will inhibit cracking of the drape.
In one embodiment, after application of the initial poly-
meric layer, a second, preferably thinner, layer is applied
thereto. Additional amounts of cyanoacrylate adhesive com-
position can be applied as needed to maintain an unbroken
coating covering over surface skin areas.
Application is conducted under conditions wherein the
polymeric drape preferably has a thickness of no more than
about 1 millimeter and, more preferably, the polymer layer
has a thickness of from about 2 to about 500 microns and
still more preferably from about 20 to about 100 microns. If
thinner polymeric drapes are desired, then the polymeric
drape should have a thickness of from about 2 to about 50
microns and preferably from 10 to 40 microns. The amount
of cyanoacrylate composition applied to a unit area of skin
to obtain such thicknesses is well within the skill of the art.
Once the polymeric surgical incise drape is formed over
the surgical incision site (which as defined above includes
the areas adjacent to the incision site), the polymeric surgical
incise drape can then optionally be overdraped with sterile
towels and sheets. In this optional embodiment, such towels
and sheets are laid over (i.e., overdrape) the surgical incision
drape to define a limited field of the surgical incise drape in
which the actual incision is to be made and the subsequent
operation is to be conducted.
In either case, the surgical incision is made through the
polymeric surgical incise drape. Any conventional incision
can be made including those created by needles, knives
(including surgical knives and surgical cautery knives),
lasers, trocar, and the like. The particular incision made is
not critical and is, of course, made relative to why the
incision is created (e.g., surgery).
Once the incision is made, the surgery or other procedure
is conducted using conventional methods. When surgery is
conducted, upon completion of the surgery, the surgical
wound is closed by conventional methods. In one
embodiment, however, closure of the epidermal or dermal
layer of the surgical wound can be accomplished by appli-
cation of cyanoacrylate adhesive composition over the
joined opposed skin sections and maintaining skin closure
until the cyanoacrylate has polymerized.
The size and thickness of the polymeric drape formed
onto the skin surface area can be readily controlled by the
amount and viscosity of cyanoacrylate adhesive composi-
tion packaged in a single dose product or by use of a multiple
use dispenser which governs the amount of material applied
onto a unit area of surface skin. In this regard, the dispenser
described by Otake, U.S. Pat. No. 4,958,748, which is
incorporated by reference in its entirety, is one example of
a dispenser which dispenses the cyanoacrylate adhesive
5,807,563
9
composition in a controlled dropwise manner. Other meth-
ods for the controlled dispersement of the cyanoacrylate
adhesive include, by Way of example, a spray applicator,
brush, Wipe, swab or solid paddle applicator, applicators for
repeated and intermittent use of the cyanoacrylate compo-
sition and the like.
In applicators, the cyanoacrylate composition is stored at
ambient conditions and can be provided in sterile form.
Because the cyanoacrylate polymer layer is Waterproof,
the patient is not prevented from bathing or being bathed and
other activities involving exposure to Water during the
period the polymer layer protects the surgical incision site
provided a further application of the cyanoacrylate compo-
sition is made over the incision site.
Compositions
The cyanoacrylate compositions comprising the polymer-
izable cyanoacrylate esters are prepared by conventional
methods of mixing the appropriate components until
homogenous.
The specific viscosity of these compositions depends, in
part, on the intended application of the composition. For
example, relatively low viscosities are often preferred Where
application is to be made to a large surface area (e.g.,
abdominal surfaces). This preference results from the fact
that those forms are less viscous and, accordingly, will
permit more facile large surface area application of a thin
application. Contrarily, Where application is to be made to a
specific position on the skin (e.g., elbow surfaces, knee
surfaces and the like), higher viscosity compositions, includ-
ing those containing thixotropic materials, are preferred to
prevent “running” of the compositions to unintended loca-
tions.
Accordingly, these compositions have a viscosity of from
about 2 to 50,000 centipoise at 20° C. Preferably the less
viscous compositions have a viscosity of from about 2 to
1,500 centipoise at 20° C. More preferably, the cyanoacry-
late ester employed in these compositions is almost entirely
in monomeric form and the composition has a viscosity of
from about 5 to about 500 centipoise at 20° C.
Athickening agent is optionally employed to increase the
viscosity of the composition, which thickening agent is any
biocompatible material which increases the viscosity of the
composition. Suitable thickening agents include, by Way of
example, polymethyl methacrylate (PMMA) or other pre-
formed polymers soluble or dispersible in the composition,
a suspending agent such as fumed silica and the like with
PMMA being preferred. Fumed silica is particularly useful
in producing a gel for topical application having a viscosity
of from about 1500 to 50,000 centipoise at 20° C. Suitable
thickening agents for the compositions described herein also
include a partial polymer of the alkyl cyanoacrylate as
disclosed in U.S. Pat. Nos. 3,654,2398 and 4,038,345” both
of which are incorporated herein by reference in their
entirety.
Thickening agents are deemed to be biocompatible if they
are soluble or dispersible in the composition and are com-
patible with the skin as measured by the lack of moderate to
severe skin irritation.
The cyanoacrylate adhesive compositions preferably
include a biocompatible plasticizer and such plasticizers are
preferably included in the composition from about 10 to 30
Weight percent and more preferably from about 18 to 25
Weight percent based on the total Weight of the composition
absent any antimicrobial agent.
Additionally, the cyanoacrylate compositions described
herein preferably include a polymerization inhibitor in an
10
15
20
25
30
35
40
45
50
55
60
65
10
effective amount to inhibit premature polymerization of the
composition during storage. In a particularly preferred
embodiment, this inhibitor is sulfur dioxide which is
employed at from about 50 to 500 ppm, preferably 200 to
500 ppm, based on the total Weight of the composition
absent any antimicrobial agent. Other preferred polymeriza-
tion inhibitors include glacial acetic acid, free radical inhibi-
tors (e.g., hydroquinones) and the like which can be used
alone or in combination with SO2.
The polymerizable cyanoacrylate ester compositions may
additionally contain one or more optional additives such as
colorants, perfumes, antidiffusion agents, rubber modifiers,
modifying agents, etc. In practice, each of these optional
additives should be both miscible and compatible with the
cyanoacrylate composition and the resulting polymer. Com-
patible additives are those that do not prevent the use of the
cyanoacrylates in the manner described herein.
In general, colorants are added so that the polymer layer
formed on the skin will contain a discrete and discernable
color. Perfumes are added to provide a pleasant smell to the
formulation. Rubber modifiers are added to further enhance
the flexibility of the resulting polymer layer. The amount of
each of these optional additives employed in the composi-
tion is an amount necessary to achieve the desired effect.
Preferred cyanoacrylate compositions useful in the prac-
tice of this invention are also disclosed by Greff, et al., U.S.
Pat. No. 5,480,935, which application is incorporated herein
by reference in its entirety.
In a particularly preferred embodiment, the cyanoacrylate
adhesive composition further comprises an antimicrobially
effective amount of a compatible antimicrobial agent. Such
compositions preferably comprise from about 1 to about 40
and preferably 5 to 30 Weight percent of the compatible
antimicrobial agent either as a solution or as a suspension
based on the total Weight of the composition. Compatible
antimicrobial agents are those which are either soluble or
suspendable in the cyanoacrylate composition, which do not
cause premature polymerization of the cyanoacrylate
composition, which do not prevent polymerization of the
cyanoacrylate composition when applied to mammalian
skin, and which are compatible with the intended use
including biocompatibility with the patient’s skin.
In a particularly preferred embodiment, the compatible
antimicrobial agent comprises a complex of iodine mol-
ecules with a biocompatible polymer. Such complexes are
Well known in the art and the resulting complex typically
comprises both available iodine and iodide anions. These
complexes, on contact with mammalian skin, provide for a
source of antimicrobial iodine. In any event, such complexes
are employed only as starting materials herein and, by
themselves, do not form a part of this invention. Suitable
biocompatible polymers include, by Way of example only,
polyvinylpyrrolidone polymer Which, when complexed with
iodine, is also referred to under the common name of
povidone-iodine available from BASF, Mt. Olive, N.J.,
USA. When povidone-iodine is employed in the cyanoacry-
late composition, it is preferably from about 5 to about 40
Weight percent and more preferably from about 10 to 25
Weight percent is added to the cyanoacrylate composition
based on the total Weight of the composition.
Cyanoacrylate compositions comprising, for example,
povidone-iodine are described by Greff, et al., U.S. Pat. U.S.
Pat. No 5,684,042 issued Nov. 4, 1997 and entitled
“Cyanoacrylate Compositions Comprising an Antimicrobial
Agent” which patent is incorporated herein by reference in
its entirety.
5,807,563
11
Other suitable antimicrobial agents include complexes of
iodine molecules with copolymers of vinylpyrrolidone and
vinyl acetate, copolymers of vinylpyrrolidone and vinyl
acetate cross-linked with polyisocyanates, copolymers of
vinylpyrrolidone and vinyl functionalities, polymers of pyr-
rolidone and the like. Preferably, however, the iodine con-
taining polymer is Povidone Iodine which is commercially
available from a number of sources.
The use of a compatible antimicrobial agent in the com-
position permits the agent to be released from the polymeric
drape thereby reducing microbial growth under the drape
during surgery. Additionally, since the drape is maintained
over the surgical incision site for 2-4 days after surgery, the
release of antimicrobial agent further provides post-surgical
anti-infection benefits.
Utility
The methods described herein are useful in forming a
polymeric surgical incise drape over the surgical incision
site of a mammalian patient. The polymeric drape finds
particular utility in inhibiting microbial contamination of the
incision during surgeries conducted on such patients. Such
mammalian patients preferably include humans as well as
domestic animals such as horses, cows, dogs, sheep, cats,
etc. The maintenance of the polymeric film over the surgical
incision after completion of the surgery is expected to reduce
the incidence of infection by inhibiting microbial contami-
nation of the incision.
The following examples illustrate certain embodiments of
the invention but is not meant to limit the scope of the claims
in any way.
EXAMPLE 1
This example illustrates how a surgical incise drape
formed in the manner of this invention could be used during
surgery. In this example, an abdominal surgical incision is to
be made through a surgical incise drape of an adult human
male and subsequent bladder surgery conducted through the
incision site.
Specifically, an adult human male (age 58) diagnosed with
bladder cancer is scheduled for surgery. The patient, after
thorough cleaning, is placed and secured on an operating
table and anesthetized. Shaving of the surgical incision area
can be performed if such is deemed necessary by the
attending surgeon. The patient then undergoes a five minute
abdominal scrub using cleansing pads and an iodine based
cleansing solution such as ethanolic povidone-iodine. After
the surgical scrub, the abdomen is thoroughly rinsed with
sterile distilled water. An antimicrobial solution of iodine is
then applied to the same area and allowed to dry.
At this time, an antimicrobial cyanoacrylate composition
comprising 73% by weight butyl cyanoacrylate, 17% by
weight dioctylphthalate, 10% povidone iodine and 200 parts
per million sulfur dioxide (each based on the total weight of
the composition) is applied to an area of approximately 20
centimeters by 30 centimeters with the proposed incision
site to be located in the center of this area. The composition
is allowed to thoroughly cure (~60 seconds) whereupon a
coherent, durable and flexible surgical incise drape is formed
over the applied area. This area is then draped with standard
sterile surgical drapes made of a waterproof paper material
to create a surgical field. The surgical field defines an area
of approximately 10 centimeters by 20 centimeters at
approximately the center of the surgical incise drape. An
incision is then made through the surgical incise drape in this
surgical field by a surgical knife and the bladder is removed
10
15
20
25
30
35
40
45
50
55
60
65
12
uneventfully. Afterwards, the peritoneum, fascia and subcu-
taneous layers are closed with standard absorbable surgical
sutures. The skin is then closed with a standard running skin
suture or staples.
At this time, the sterile surgical drapes made of a water-
proof paper material are removed from the patient leaving
only the surgical incise drape which is strongly adherent to
the skin. A surgical dressing is applied over the incision site
and the patient is awakened from the anesthetic agent. The
surgical dressing is checked every 4 hours for signs of
seepage and changed daily until patient is discharged
(typically 2-3 days after surgery).
The surgical incise drape formed by the film of
cyanoacrylate polymer sloughs off naturally over 1-4 days
after surgery as the patient’s outer layer of skin naturally
sloughs off without any complications. The povidone-iodine
in the film is antimicrobial thereby providing an antimicro-
bial effect during this period.
EXAMPLE 2
This example illustrates how a surgical incise drape
formed in the manner of this invention could be used during
arthroscopic surgery correcting a partial medial collateral
ligament tear to a patient’s knee. Because of the conforma-
tion of the knee, a higher viscosity cyanoacrylate composi-
tion is desirable in order to prevent “running” of the com-
position prior to formation of the polymeric drape. In this
example, three separate surgical incisions are made creating
portals through which cannulas a replaced through a poly-
meric surgical incise drape formed in the manner of this
invention over the knee and subsequent repair of the torn
ligaments is conducted through these cannulas.
Specifically, an adult female (age 36) diagnosed with a
torn medial collateral ligament of the right knee is scheduled
for outpatient surgery to arthroscopically repair the torn
ligament. The patient, after thorough cleansing, is placed
and secured on an operating table, and is anesthetized. The
patient then undergoes a five minute scrub using cleansing
pads and an iodine based cleansing solution such as ethan-
olic povidone-iodine. After the surgical scrub, the knee i s
thoroughly rinsed with sterile distill ed water. An antimi-
crobial solution of iodine is then applied to the same area
and allowed to dry.
At this time, a viscous antimicrobial cyanoacrylate com-
position comprising 68% by weight butyl cyanoacrylate, 5
weight percent polymethyl methacrylate, 17% by weight
dioctylphthalate, 10% povidone iodine and 200 parts per
million sulfur dioxide (each based on the total weight of the
composition) is applied to the entire knee area extending
approximately 5 centimeters above and below the knee joint
with the proposed trocar incision sites to be located within
the boundaries of this area. The composition is allowed to
thoroughly cure (-60 seconds) whereupon a coherent,
durable and flexible surgical incise drape is formed over the
applied area. This area is then draped with standard sterile
surgical drapes made of a waterproof paper material to
create a surgical field within the surgical incise drape. Three
separate incisions are made into the knee joint through the
surgical incise drape in this surgical field and three separate
cannulas are placed in a position such that the medial
collateral ligament tear is repaired uneventfully. Afterwards,
the skin is closed with a separate cyanoacrylate composition
comprising n-butyl cyanoacrylate and 100 ppm sulfur diox-
ide that bonds the skin together. The cyanoacrylate poly-
meric film naturally sloughs off within 1-4 days after
formation. The povidone-iodine in the film renders the film
5,807,563
13
antimicrobial thereby providing an antimicrobial effect dur-
ing this period.
EXAMPLE 3
The following example was conducted to ascertain the
antimicrobial effect of a cyanoacrylate polymer film com-
prising PVP-iodine.
A. Preparation of the Inoculum
Specifically, the surfaces of two TSA plates, 100>
Coments go here:
- Log in to post comments