Chlorhexidine Compared with Povidone-Iodine Solution for Vascular Catheter–Site Care: A Meta-Analysis
Chlorhexidine Compared with Povidone-Iodine Solution for Vascular Catheter–Site Care: A Meta-Analysis
Folder:
Journal:
Year:
Abstract:
Bloodstream infections related to use of catheters, particularly central-line catheters, are an important cause of patient morbidity, mortality, and increased health care costs. This study evaluated the efficacy of skin disinfection with chlorhexidine gluconate compared with povidone-iodine solution in preventing catheter-related bloodstream infection.
Type of document:
Language:
Article
Chlorhexidine Compared with Povidone-Iodine Solution for Vascular
Catheter–Site Care: A Meta-Analysis
Nathorn Chaiyakunapruk, PharmD, PhD; David L. Veenstra, PharmD, PhD; Benjamin A. Lipsky, MD; and Sanjay Saint, MD, MPH
Purpose: Bloodstream infections related to use of catheters, particularly central-line catheters, are an important cause of patient
morbidity, mortality, and increased health care costs. This study
evaluated the efficacy of skin disinfection with chlorhexidine gluconate compared with povidone-iodine solution in preventing
catheter-related bloodstream infection.
Data Sources: Multiple computerized databases (1966 to 2001),
reference lists of identified articles, and queries of principal investigators and antiseptic manufacturers.
Study Selection: Randomized, controlled trials comparing chlorhexidine gluconate with povidone-iodine solutions for cathetersite care.
Data Extraction:
Using a standardized form, two reviewers
abstracted data on study design, patient population, intervention,
and incidence of catheter-related bloodstream infection from all
included studies.
I
ntravascular catheters are commonly used in caring for
hospitalized patients but can lead to serious infectious
complications (1). Catheter-related bloodstream infection is associated with increased morbidity, mortality,
length of hospitalization, and medical costs (2– 6). Use
of an antiseptic solution for skin disinfection at the catheter insertion site helps prevent catheter-related infections. Povidone-iodine solution is the most commonly
used agent for this purpose (7, 8).
Recently, several studies have compared the efficacy
of povidone-iodine with that of chlorhexidine gluconate
solutions for reducing vascular catheter–related infections (7, 9 –14; Knasinski V, Maki DG. A prospective,
randomized, controlled trial of 1% chlorhexidine 75%
alcohol vs. 10% povidone iodine for cutaneous disinfection and follow-up site care with central venous and
arterial catheters [Presented paper]. San Diego: National
Association of Vascular Access Network Conference;
2000). Unfortunately, because few clinical events have
been observed in individual studies, it remains unclear
which antiseptic solution is best, both statistically and
clinically, for reducing the risk for catheter-related
bloodstream infection, particularly in patients with central-line catheters.
792 © 2002 American College of Physicians–American Society of Internal Medicine
Data Synthesis:
Eight studies involving a total of 4143 catheters met the inclusion criteria. All studies were conducted in a
hospital setting, and various catheter types were used. The summary risk ratio for catheter-related bloodstream infection was 0.49
(95% CI, 0.28 to 0.88) in patients whose catheter sites were
disinfected with chlorhexidine gluconate instead of povidoneiodine. Among patients with a central vascular catheter, chlorhexidine gluconate reduced the risk for catheter-related bloodstream
infection by 49% (risk ratio, 0.51 [CI, 0.27 to 0.97]).
Conclusions: These results suggest that incidence of bloodstream infections is significantly reduced in patients with central
vascular lines who receive chlorhexidine gluconate versus povidone-iodine for insertion-site skin disinfection. Use of chlorhexidine gluconate is a simple and effective means of reducing vascular catheter–related infections.
Ann Intern Med. 2002;136:792-801.
For author affiliations, see end of text.
www.annals.org
We sought to aid clinical decision making by evaluating the effectiveness of chlorhexidine gluconate versus povidone-iodine as a skin disinfectant for cathetersite care. We performed a meta-analysis of all available
published and unpublished studies comparing chlorhexidine gluconate with povidone-iodine solution for
vascular catheter–site care.
METHODS
Study Selection
We manually searched Index Medicus (1960 to
1965) and electronically searched MEDLINE (1966 to
2001), CINAHL: Nursing and Allied Health (1982 to
2001), Doctoral Dissertation Abstracts (1861 to 2001),
International Pharmaceutical Abstracts (1970 to 2001),
EMBASE, Lexis–Nexus, Web of Sciences, and Cochrane Library databases for publications in any language.
For our search strategy, we used the Medical Subject
Headings chlorhexidine and catheterization and the exploded key words chlorhexidine and catheter. We restricted the searches to clinical trials. To ensure that our
search would be thorough, we consulted a research librarian at the University of Washington. To identify
Antiseptic for Catheter-Site Care: A Meta-Analysis
additional original studies, we reviewed the reference
lists of the retrieved articles and any identified review
articles. Studies presented at recent scientific meetings in
the area of infection control were also identified by reviewing meeting programs and published meeting proceedings and by attending medical meetings on related
topics. We contacted the manufacturer of chlorhexidine
gluconate solution, the corresponding authors of relevant studies, and experts in the field to inquire about
possible additional studies.
To be included in the meta-analysis, a study needed
1) to be a randomized trial comparing any type of chlorhexidine gluconate solution with a povidone-iodine solution for vascular catheter–site care and 2) to report the
incidence of catheter colonization or catheter-related
bloodstream infection with sufficient data to calculate
the risk ratio.
Context
Intravascular catheter–related bloodstream infection is an
important and potentially avoidable cause of morbidity.
Various antiseptic solutions for skin disinfection and catheter-site care may help prevent catheter-related infections.
Contribution
This article summarizes data from eight randomized trials
that compared antiseptic solutions.
Approximately 1% of the patients with chlorhexidine gluconate disinfectant developed bloodstream infections from
intravascular catheters. In the patients with disinfection by
povidone-iodine, the rate was 2% (risk ratio, 0.49 [95%
CI, 0.28 to 0.88]).
Implications
Chlorhexidine gluconate is more effective than povidoneiodine for intravascular catheter–site care. It is also more
expensive.
–The Editors
Outcome Measures
The primary outcome was catheter-related bloodstream infection, which we defined as isolation of the
same organism (that is, identical species with the same
antibiograms) from a peripheral blood culture and a
semiquantitative or quantitative culture of a catheter
segment. Our secondary outcome, catheter colonization,
was defined as significant growth of microorganisms
from a catheter segment, according to quantitative
(Ͼ1000 colony-forming units [CFUs] per mL) or semiquantitative (Ͼ15 CFU) culture techniques (15, 16).
Data Extraction
Using a standardized data form, two investigators
independently abstracted data on the size of the study
sample, type of patient population, type of vascular
catheter used, type of antiseptic used, anatomic site of
insertion, use of catheter exchange with guide wire, concurrent use of other interventions, and incidence of
catheter colonization and catheter-related bloodstream
infection. We also evaluated the following methodologic
components of each study: randomization procedure, extent of blinding, and description of eligible participants. The authors of studies that did not contain
sufficient data were contacted for additional information.
www.annals.org
Article
Statistical Analysis
We separately analyzed the incidences of catheter
colonization and catheter-related bloodstream infection.
The summary risk ratios and 95% CIs were calculated
by using the DerSimonian and Laird method under a
random-effects model (17). A statistical test of heterogeneity was performed by using the Mantel–Haenszel
method (18). To explore potential clinical sources of
heterogeneity, we conducted sensitivity analyses according to characteristics of the study, the study participants,
the types of catheters used, outcome definitions, and
concentrations of antiseptics used. We explored publication bias using the funnel-plot method by graphing the
effect size of trials on the horizontal axis and the number
of participants in each trial on the vertical axis (19);
asymmetry in the funnel plot suggested publication bias.
Because some studies allowed patients to receive
more than one vascular catheter during the study period,
the within-patient correlation could underestimate the
standard error of the effect measure. To investigate this
effect, we inflated the variance of the risk ratio for
each study by multiplying it by the average number of
catheters per patient (20). To perform all statistical analyses, we used Stata software, version 6.0 (Stata Corp.
College Station, Texas), by employing the command
“METAN.”
4 June 2002 Annals of Internal Medicine Volume 136 • Number 11 793
Article
Antiseptic for Catheter-Site Care: A Meta-Analysis
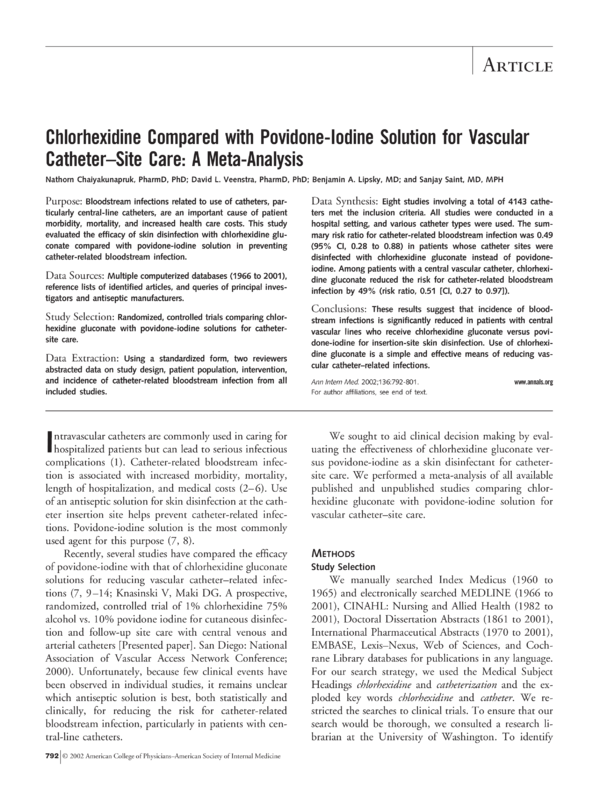
Figure 1. Trial flow depicting the selection process of
studies included in the meta-analysis.
view of the full manuscripts of potentially relevant articles, identified 6 published studies that met our inclusion criteria. Of the 296 remaining studies, 285 were
excluded because chlorhexidine gluconate was not used
for catheter-site care (n ϭ 268), use of the disinfectants
was not determined by random allocation (n ϭ 13), povidone-iodine was not used as a comparator (n ϭ 2), or
colonization or catheter-related bloodstream infection
was not recorded (n ϭ 2). The other 11 excluded studies were duplicate studies retrieved from different databases. In addition to the 6 studies identified from
searches, 1 published abstract (9) and 1 published study
(10) were identified from the reference list of a review
article (21). Thus, our meta-analysis comprised 8 total
studies. Studies were reviewed by two investigators, and
there were no discrepancies in the abstracted data.
Study Characteristics
RCT ϭ randomized, controlled trial.
RESULTS
Study Selection
We located 302 articles from our manual and computerized searches (Figure 1). Reviews of the titles and
abstracts from the computerized search, followed by re794 4 June 2002 Annals of Internal Medicine Volume 136 • Number 11
Table 1 shows the characteristics of the eight included studies. These trials used 4143 catheters (1493
central venous, 1361 peripheral venous, 704 peripheral
arterial, 395 pulmonary arterial, 75 peripherally inserted
central venous, 62 introducer sheaths, and 53 hemodialysis). Five studies included only patients from intensive care units (7, 9, 11, 12, 14); three studies included
patients from any unit in the hospital (10, 13; Knasinski
V, Maki DG [Presented paper]). One study was a multicenter clinical trial (10). Among the included studies
that reported patient age, the average age ranged from
50 to 65 years (7, 10 –12, 14). The mean duration of
catheterization for the chlorhexidine gluconate and povidone-iodine groups was similar in all studies that provided this information, except one in which the chlorhexidine gluconate group was catheterized longer (9.9
vs. 5.9 days) (14). There was no significant difference in
the anatomic sites (such as subclavian or femoral) in
which catheters were inserted between the chlorhexidine
gluconate and povidone-iodine groups. One study allowed catheter exchange via a guide wire (7). Only one
study noted adverse effects from the use of either antiseptic solution: Maki and colleagues (7) found erythema
at the insertion site in 28.3% of catheters in the povidone-iodine group and in 45.3% of catheters in the
chlorhexidine gluconate group (P Ͻ 0.001). However,
there was no statistically significant difference in erywww.annals.org
Antiseptic for Catheter-Site Care: A Meta-Analysis
thema among these two groups and patients whose sites
were disinfected with alcohol (7).
The included studies used several formulations of
chlorhexidine gluconate. Five studies (10, 13, 14; Knasinski V, Maki DG [Presented paper]) used an alcoholic
solution, and three studies (7, 9, 11) used an aqueous
solution. All studies used 10% povidone-iodine solution
for the control group. However, only one study specified
the sequence of applications of 70% alcohol and 10%
povidone-iodine (13). Five studies clearly described their
procedures for care of the catheter site (7, 10 –12, 14);
in these studies, the dressing was changed and the insertion site was typically cleansed every 48 to 72 hours (7).
Sterile gauze was used for dressing in three studies (7,
11, 14); meanwhile, one study used semiocclusive dressing (12) and another study used opaque and transparent
dressings (10). Four studies (10, 11, 13; Knasinski V,
Maki DG [Presented paper]) specified that antibiotic
ointments were not used; three studies (10, 13; Knasinski V, Maki DG [Presented paper]) specifically indicated
that no antimicrobial-impregnated catheters were allowed.
Five studies (7, 9, 13, 14; Knasinski V, Maki DG
[Presented paper]) cultured intravascular catheter segments by using the roll-plate semiquantitative method
(16), two studies (11, 12) used the quantitative culture
method (15), and one study defined catheter colonization by either method (10). All studies evaluating catheter-related bloodstream infection as an outcome required the recovery of the same microbial species from
both the catheter segment and a blood culture. In addition, two studies (14; Knasinski V, Maki DG [Presented
paper]) required confirmation by molecular subtyping,
five studies (7–10, 14; Knasinski V, Maki DG [Presented paper]) required no other sources of infection, and
five (7, 9 –12) required the presence of clinical signs or
symptoms of infection (Table 1). All studies provided
sufficient information to calculate the incidence of catheter colonization and catheter-related bloodstream infection except for the study by LeBlanc and Cobett (13),
which provided data on catheter colonization only.
The unit of randomization was the patient in all
included studies, except for two studies that used random assignment based on catheters (9, 12). For these
latter two studies, the average catheter-to-patient ratio
(that is, the number of catheters inserted during hospitalization in a particular patient) was 1.83 and 2.41,
www.annals.org
Article
respectively. Four studies reported the randomization
procedure (10, 11, 13, 14), which was found adequate
on reviewer assessment. Only one study blinded investigators to antiseptic solution being used (13). Patient
eligibility criteria were clearly described in all studies
except three (9, 13; Knasinski V, Maki DG [Presented
paper]).
Catheter-Related Bloodstream Infection and Catheter
Colonization
Risk for catheter colonization and catheter-related
bloodstream infection were significantly lower in the
chlorhexidine gluconate group than in the povidoneiodine group (Table 2). The summary risk ratio for
catheter colonization for all vascular catheters in the
chlorhexidine gluconate compared with the povidoneiodine group was 0.49 (95% CI, 0.31 to 0.71). The
summary risk ratio for catheter-related bloodstream infection for all vascular catheters was 0.49 (CI, 0.28 to
0.88), indicating a significantly reduced risk in patients
using chlorhexidine gluconate (Figure 2). The pooled
proportions of colonization and catheter-related bloodstream infection in the povidone-iodine group were
0.139 (CI, 0.087 to 0.191) and 0.0216 (CI, 0.0124 to
0.0307), respectively. The absolute risk reduction was
7.1% for colonization and 1.1% for catheter-related bloodstream infection. The test for heterogeneity of treatment
effect was significant for catheter colonization (P Ͻ 0.001)
but not for catheter-related bloodstream infection
(P Ͼ 0.2). There was no evidence of publication bias, as
indicated by the symmetrical shape of the funnel plot.
Sensitivity Analyses
Sensitivity analyses performed to investigate possible
sources of heterogeneity in the studies examining catheter colonization showed that the trial by Humar and
colleagues (14) was the predominant source. This was
the only study in which the incidence of catheter colonization in the chlorhexidine gluconate group was
higher than that in the povidone-iodine group. The increased risk for catheter colonization in the chlorhexidine gluconate group probably resulted from the longer
mean duration of catheterization compared with the povidone-iodine group (9.9 vs. 5.2 days) (14) among patients whose catheter segment was available for a semiquantitative culture. When this study was excluded from
4 June 2002 Annals of Internal Medicine Volume 136 • Number 11 795
Article
Antiseptic for Catheter-Site Care: A Meta-Analysis
Table 1. Characteristics of Studies Comparing Chlorhexidine Gluconate Solutions with Povidone-Iodine Solutions for
Vascular Catheter–Site Care*
Study (Reference), Year
Antiseptic CHG
Solution
Patient
Population
Catheters and Patients, n/n
Mean Catheter Duration, d
CHG Group
Povidone-Iodine
Group†
CHG Group
Povidone-Iodine
Group†
Maki et al. (7), 1991
2% aqueous
ICU
214/214
227/227
5.3
5.3
Sheehan et al. (9), 1993
2% aqueous
ICU
169/94
177/95
NA
NA
Meffre et al. (10), 1995‡
0.5% alcohol
Any hospital unit
568/568
549/549
1.6
1.6
Mimoz et al. (11), 1996
Biseptine§
ICU
170/NA
145/NA
4.5
3.9
Legras et al. (12), 1997
0.5% alcohol
ICU
208/88
249/102
10
10
LeBlanc and Cobett (13), 1999‡
0.5% alcohol
Any hospital unit
83/83
161/161
1.6
1.7
Humar et al. (14), 2000
0.5% alcohol
ICU
193/193
181/181
5.3
6.3
Knasinski and Maki, 2000‡¶
1% alcohol
Any hospital unit
349/349
500/500
NA
NA
* CFU ϭ colony-forming unit; CHG ϭ chlorhexidine gluconate; ICU ϭ intensive care unit; NA ϭ not available.
† All studies used 10% povidone-iodine solution.
‡ Author provided additional information.
§ Biseptine (Nicholas, Gaillard, France) consists of 0.25% CHG, 0.025% benzalkonium chloride, and 4% benzyl alcohol.
Required one of the following symptoms: fever, erythema, heat at the site, pain.
¶ Knasinski V, Maki DG. A prospective, randomized, controlled trial of 1% chlorhexidine 75% alcohol vs. 10% povidone iodine for cutaneous disinfection and follow-up
site care with central venous and arterial catheters [Presented paper]. San Diego: National Association of Vascular Access Network Conference; 2000.
our analysis, the P value for the test of heterogeneity
increased from less than 0.001 to greater than 0.2. Analysis of the other seven studies produced a summary risk
ratio for catheter colonization of 0.43 (CI, 0.33 to
0.55). After the study by Humar and colleagues (14)
was excluded, the summary risk ratio for catheter-related
bloodstream infection (0.45 [CI, 0.23 to 0.85]) was similar to that found when all studies were included. Accounting for increased variance due to possible withinpatient correlation led to similar point estimates and CIs
for catheter colonization (risk ratio, 0.49 [CI, 0.31 to
0.78]) and catheter-related bloodstream infection (risk
ratio, 0.50 [CI, 0.28 to 0.91]).
In all subgroup analyses, the overall relative risk reductions with chlorhexidine gluconate compared with
povidone-iodine remained approximately 50% for cath796 4 June 2002 Annals of Internal Medicine Volume 136 • Number 11
eter colonization and for catheter-related bloodstream
infection. When we excluded the study that allowed
catheter exchange over a guide wire, the results (risk
ratio, 0.53 [CI, 0.33 to 0.85] for catheter colonization
and 0.54 [CI, 0.29 to 0.98] for catheter-related bloodstream infection) were still consistent with our main
findings. Analysis of studies using chlorhexidine alcohol
solutions produced a summary risk ratio of 0.57 (CI,
0.35 to 0.94) for catheter colonization and 0.52 (CI,
0.28 to 0.96) for catheter-related bloodstream infection.
When only central vascular catheters (that is, nontunneled central venous catheters, pulmonary arterial
catheters, and peripherally inserted central venous catheters) were included in the analysis, the results were similar (summary risk ratio, 0.52 [CI, 0.29 to 0.95] for
catheter colonization and 0.51 [CI, 0.27 to 0.97] for
www.annals.org
Antiseptic for Catheter-Site Care: A Meta-Analysis
Table 1—Continued
Article
the definition of catheter-related bloodstream infection,
the summary risk ratio was 0.50 (CI, 0.26 to 0.96).
Outcome Definitions
Catheter
Colonization
Catheter-Related Bloodstream Infection
Semiquantitative
(Ͼ15 CFU)
Same organism or species matched between blood
and catheter segment culture; no other source
of infection; clinical symptoms of bloodstream
infection
Same organism or species matched between blood
and catheter segment culture; no other source
of infection; clinical symptoms of bloodstream
infection
Local or clinical symptoms of bloodstream
infection or same organism or species matched
between blood and catheter segment culture;
no other source of infection
Same organism or species matched between blood
and catheter segment culture; clinical symptoms
of bloodstream infection
Same organism or species matched between blood
and catheter segment culture; clinical symptoms
of bloodstream infection
NA
Semiquantitative
(Ͼ15 CFU)
Semiquantitative
(Ͼ15 CFU) or
quantitative
(Ͼ103 CFU/mL)
Quantitative
(Ͼ103 CFU/mL)
Quantitative
(Ͼ103 CFU/mL)
Semiquantitative
(Ͼ15 CFU)
Semiquantitative
(Ͼ15 CFU)
Semiquantitative
(Ͼ15 CFU)
Same organism or species matched between blood
and catheter segment culture; same organism
confirmed by molecular subtyping; no other
source of infection
Same organism or species matched between blood
and catheter segment culture; same organism
confirmed by molecular subtyping; no other
source of infection
catheter-related bloodstream infection). Likewise, an
analysis including only noncentral catheters revealed
similar results (risk ratio, 0.39 [CI, 0.21 to 0.71] for
catheter colonization and 0.45 [CI, 0.05 to 3.77] for
catheter-related bloodstream infection). In studies that
included only patients hospitalized in intensive care
units, the summary risk ratio for disinfection by chlorhexidine gluconate was 0.53 (CI, 0.27 to 1.03) for
catheter colonization and 0.52 (CI, 0.23 to 1.17) for
catheter-related bloodstream infection.
Analysis of studies that required clinical symptoms
(for the definition of catheter-related bloodstream infection or as the indication for drawing blood cultures)
yielded a summary risk ratio for catheter-related bloodstream infection of 0.53 (CI, 0.22 to 1.27). In the studies for which catheter-related bloodstream infection required identical antibiograms or molecular subtyping,
the summary risk ratio for chlorhexidine gluconate was
0.52 (CI, 0.27 to 1.02). In an analysis of the studies in
which absence of other sources of infection was part of
www.annals.org
DISCUSSION
Use of chlorhexidine gluconate solution for care of
catheter sites is significantly more effective than use of
povidone-iodine solution for preventing vascular catheter–related infections. We estimate that for every 1000
catheter sites disinfected with chlorhexidine gluconate
rather than povidone-iodine, 71 episodes of catheter colonization and 11 episodes of catheter-related bloodstream infection would be prevented.
The summary risk reduction for catheter-related
bloodstream infection in the main analysis and the sensitivity analyses suggests that chlorhexidine gluconate solution reduces the risk for catheter-related bloodstream
infection by approximately 50%. This reduction remained statistically significant even when only central
vascular catheters were included. The implications of
such a reduction are substantial because patients requiring central vascular catheters are typically at high risk for
this costly complication (22–24). The magnitudes of the
risk reductions in the subgroup analyses were similar to
those in the main analysis. The failure to find a significant difference in some subgroup analyses is probably
due to the low incidence of clinical events (for example,
with peripheral lines) and small sample sizes.
Our study has several limitations that stem from the
designs of the individual trials. First, in studies with
multiple catheters per patient, the effects measured for
the same patient are likely to be correlated. The resulting within-patient correlation causes an underestimation
of the standard error of the benefits of chlorhexidine
gluconate solution. A sensitivity analysis in which the
variance of the studies was increased affected the results
only slightly.
Second, several types of chlorhexidine gluconate solution were used in the individual trials, including 0.5%
or 1% chlorhexidine gluconate alcohol solution and
0.5% or 2% chlorhexidine gluconate aqueous solution.
All of these solutions provide a concentration of chlorhexidine gluconate that is higher than the minimal inhibitory concentrations for most nosocomial bacteria
and yeast (7). Subset analyses of aqueous and nonaqueous solutions showed similar effect sizes, but only the
subset analysis of the five studies that used alcoholic
4 June 2002 Annals of Internal Medicine Volume 136 • Number 11 797
Article
Antiseptic for Catheter-Site Care: A Meta-Analysis
Table 2. Results of Studies Comparing Chlorhexidine Gluconate Solutions with Povidone-Iodine Solutions for Vascular
Catheter–Site Care*
Study (Reference), Year
Catheter Colonization
Proportion of Positive Cultures
CHG Group
Catheter-Related Bloodstream Infection
RR (95% CI) Using
CHG Solution†
Povidone-Iodine
Group
CHG Group
n/n (%)
Maki et al. (7), 1991
Sheehan et al. (9), 1993
Meffre et al. (10), 1995‡
Mimoz et al. (11), 1996
Legras et al. (12), 1997
LeBlanc and Cobett (13), 1999‡
Humar et al. (14), 2000
Knasinski and Maki, 2000‡§
All studies
All studies excluding Humar et al.
5/214 (2.3)
3/169 (1.8)
9/568 (1.6)
12/170 (7.1)
19/208 (9.1)
6/83 (7.2)
36/116 (31.0)
33/349 (9.5)
21/227 (9.2)
12/177 (6.8)
22/549 (4.0)
24/145 (16.6)
31/249 (12.4)
23/161 (16.1)
27/116 (23.3)
127/500 (25.4)
Proportion of Patients with
Infection
RR (95% CI) Using
CHG Solution†
Povidone-Iodine
Group
n/n (%)
0.25 (0.10–0.66)
0.22 (0.06–0.75)
0.40 (0.18–0.85)
0.43 (0.22–0.82)
0.73 (0.43–1.26)
0.49 (0.31–0.77)
1.33 (0.87–2.04)
0.37 (0.26–0.53)
0.49 (0.31–0.71)
0.43 (0.33–0.55)
1/214 (0.4)
1/169 (0.6)
3/568 (0.5)
3/170 (1.8)
0/208 (0.0)
–
4/193 (2.1)
5/349 (1.4)
6/227 (2.6)
1/177 (0.6)
3/549 (0.5)
4/145 (2.8)
4/249 (1.6)
–
5/181 (2.8)
20/500 (4.0)
0.18 (0.02–1.46)
1.05 (0.07–16.61)
0.97 (0.20–4.77)
0.64 (0.15–2.81)
0.13 (0.01–2.45)
–
0.75 (0.20–2.75)
0.36 (0.14–0.95)
0.49 (0.28–0.88)
0.45 (0.23–0.85)
* CHG ϭ chlorhexidine gluconate; RR ϭ risk ratio.
† Risk ratio for use of chlorhexidine gluconate versus povidone-iodine.
‡ Author provided additional information.
§ Knasinski V, Maki DG. A prospective, randomized, controlled trial of 1% chlorhexidine 75% alcohol vs. 10% povidone iodine for cutaneous disinfection and follow-up
site care with central venous and arterial catheters [Presented paper]. San Diego: National Association of Vascular Access Network Conference; 2000.
solution produced a statistically significant reduction in
catheter-related bloodstream infection. Because few
studies used chlorhexidine gluconate aqueous solution,
the lack of a significant difference seen for this solution
compared with povidone-iodine solution may be a result
of inadequate statistical power.
Third, several studies defined catheter-related
bloodstream infection differently. Some studies required
the presence of clinical symptoms of bloodstream infection (7, 9 –12) or the absence of other sources of infection (7, 9, 10, 14; Knasinski V, Maki DG [Presented
paper]), whereas other studies used molecular subtyping
techniques to determine whether the organisms isolated
were identical (14; Knasinski V, Maki DG [Presented
paper]). All trials, however, required isolation of the
same organism or microbial species from a peripheral
blood culture and a culture of a catheter segment.
Fourth, none of the eight included studies reported
strategies to distinguish true bacteremia from blood culture contamination. Given that coagulase-negative
staphylococci are the most common contaminants (25),
it is possible that contaminated specimens may have
been falsely viewed as true bacteremia. In the studies
that reported the organism causing catheter-related
bloodstream infection (7, 12, 14), gram-positive cocci
798 4 June 2002 Annals of Internal Medicine Volume 136 • Number 11
caused most infections (62%); 29% of the organisms
were specifically coagulase-negative staphylococci. If it is
assumed that the same procedures were used to obtain a
peripheral blood culture in the chlorhexidine gluconate
and povidone-iodine groups, the rate of misclassification
would be similar in both groups.
The heterogeneity identified in the analysis of catheter colonization implies that these trials may have measured different treatment effects for the povidone-iodine
and chlorhexidine gluconate solutions. The source of
the heterogeneity, however, arose mainly from the study
by Humar and colleagues (14), probably as a result of
the longer mean duration of catheterization in the chlorhexidine gluconate group.
Publication bias seriously threatens the methodologic validity of meta-analyses (18). To minimize this
bias, we exhaustively searched for published and unpublished studies in any language. If publication bias were
present, the smaller trials would tend to report a greater
preventive effect because smaller trials with significant
results are more likely to be published than are smaller
studies with nonsignificant results. Our analysis, however, revealed no evidence of such a bias.
The superiority of chlorhexidine gluconate for catheter-site care has several potential explanations. First,
www.annals.org
Antiseptic for Catheter-Site Care: A Meta-Analysis
blood, serum, and other protein-rich biomaterials can
deactivate the microbicidal effect of povidone-iodine
(26, 27) but not chlorhexidine gluconate (28, 29). Second, the residual effect of chlorhexidine gluconate, defined as the long-term antimicrobial suppressive activity,
is prolonged (at least 6 hours) (30, 31), while that of
povidone-iodine is minimal (32). The superiority of
chlorhexidine gluconate compared with povidoneiodine in reducing the colony counts of coagulase-negative staphylococci has been previously shown in a study
of disinfection of peritoneal dialysis catheter sites (33).
Because most vascular catheter–related infections are
caused by gram-positive cocci, the superior bactericidal
effect of chlorhexidine gluconate against these organisms
is likely to be clinically important.
Two additional issues should be considered regarding the use of chlorhexidine gluconate for catheter-site
care. Hypersensitivity reactions have been reported with
use of central venous catheters impregnated by chlorhexidine-silver sulfadiazine and with use of chlorhexidine gluconate for bathing (34 –38). No hypersensitivity
reactions were reported by the studies in our meta-anal-
Article
ysis; however, clinicians should be alert to this and other
potential side effects, including increased erythema,
which one study (7) reported. Bacterial resistance is
another potential concern, but very few reports of resistance to chlorhexidine gluconate exist despite its widespread use for several decades (39).
Our results are somewhat generalizable. We combined clinical trials with different patient populations;
different concentrations and types of chlorhexidine gluconate solution; and different types of vascular catheters
inserted, on average, for 1 to approximately 10 days.
Thus, our results may apply to most hospitalized patients in the United States and similar health care settings. We cannot address, however, the role of chlorhexidine gluconate in preventing catheter-related
bloodstream infection in patients who are catheterized
for an average of longer than 10 days or the potential
additional benefit of chlorhexidine gluconate when an
antimicrobial catheter is used (40, 41).
Considering the progressive accumulation of studies
over the past decade supporting the efficacy of chlorhexidine gluconate in reducing catheter colonization,
Figure 2. Analysis of catheter-related bloodstream infection in studies comparing chlorhexidine gluconate and
povidone-iodine solutions for care of vascular catheter sites.
The diamond indicates the summary risk ratio and 95% CI. Studies are ordered chronologically. The size of squares is proportional to the reciprocal of
the variance of the studies. For the test for heterogeneity of treatment effect, P Ͼ 0.2. *Knasinski V, Maki DG. A prospective, randomized, controlled
trial of 1% chlorhexidine 75% alcohol vs. 10% povidone iodine for cutaneous disinfection and follow-up site care with central venous and arterial
catheters [Presented paper]. San Diego: National Association of Vascular Access Network Conference; 2000.
www.annals.org
4 June 2002 Annals of Internal Medicine Volume 136 • Number 11 799
Article
Antiseptic for Catheter-Site Care: A Meta-Analysis
why has this disinfectant not been more widely used for
catheter-site care? One reason may be the previous lack
of clear clinical evidence demonstrating the superiority
of chlorhexidine gluconate versus povidone-iodine in reducing catheter-related bloodstream infections in patients with central vascular catheters. Another reason
may be the higher cost of chlorhexidine gluconate.
However, although chlorhexidine gluconate is approximately twice as expensive as povidone-iodine, the absolute difference is relatively small (approximately $0.92
vs. $0.41 for a quantity sufficient to prepare an insertion
site for a central venous catheter). Although our metaanalysis suggests that the use of chlorhexidine gluconate
is likely to be cost-effective, or even cost saving, a formal
economic evaluation is needed.
We found that the use of chlorhexidine gluconate
rather than povidone-iodine can reduce the risk for
catheter-related bloodstream infection by approximately
50% in hospitalized patients who require short-term
catheterization. Given the extent of the benefit and the
small incremental cost, chlorhexidine gluconate should
be considered as a replacement for povidone-iodine solution, particularly in patients at high risk for catheterrelated bloodstream infection.
From Naresuan University, Pitsanuloak, Thailand; University of Washington and Veterans Affairs Puget Sound Healthcare System, Seattle,
Washington; and University of Michigan and Ann Arbor Veterans Administration Medical Center, Ann Arbor, Michigan.
Acknowledgments: The authors thank Gerard Sheehan, MD, John M.
Conly, MD, Raphaele Girard, MD, Angela LeBlanc, BSc (Hed), and
Valerie Knasinski, RN, for providing citations of additional studies or
additional information from their studies. They also thank Todd A. Lee,
PharmD, PhD, for helping with the abstraction of these studies.
Requests for Single Reprints: David L. Veenstra, PharmD, PhD, Pharmaceutical Outcomes Research and Policy Program, Department of
Pharmacy, Box 357630, University of Washington, Seattle, WA 981957630; e-mail, veenstra@u.washington.edu.
Current author addresses and author contributions are available at www
.annals.org.
References
1. Raad I. Intravascular-catheter-related infections. Lancet. 1998;351:893-8.
[PMID: 9525387]
2. Smith RL, Meixler SM, Simberkoff MS. Excess mortality in critically ill
patients with nosocomial bloodstream infections. Chest. 1991;100:164-7.
[PMID: 2060337]
800 4 June 2002 Annals of Internal Medicine Volume 136 • Number 11
3. Martin MA, Pfaller MA, Wenzel RP. Coagulase-negative staphylococcal bacteremia. Mortality and hospital stay. Ann Intern Med. 1989;110:9-16. [PMID:
2908834]
4. Haley RW, Schaberg DR, Von Allmen SD, McGowan JE Jr. Estimating the
extra charges and prolongation of hospitalization due to nosocomial infections: a
comparison of methods. J Infect Dis. 1980;141:248-57. [PMID: 6767793]
5. Pittet D, Tarara D, Wenzel RP. Nosocomial bloodstream infection in critically ill patients. Excess length of stay, extra costs, and attributable mortality.
JAMA. 1994;271:1598-601. [PMID: 8182812]
6. Arnow PM, Quimosing EM, Beach M. Consequences of intravascular catheter sepsis. Clin Infect Dis. 1993;16:778-84. [PMID: 8329510]
7. Maki DG, Ringer M, Alvarado CJ. Prospective randomised trial of povidoneiodine, alcohol, and chlorhexidine for prevention of infection associated with
central venous and arterial catheters. Lancet. 1991;338:339-43. [PMID:
1677698]
8. Clemence MA, Walker D, Farr BM. Central venous catheter practices: results
of a survey. Am J Infect Control. 1995;23:5-12. [PMID: 7762875]
9. Sheehan G, Leicht K, O’Brien M, Taylor G, Rennie R. Chlorhexidine versus
povidone-iodine as cutaneous antisepsis for prevention of vascular-catheter infection [Abstract]. In: Program and Abstracts—Interscience Conference on Antimicrobial Agents and Chemotherapy. Washington, DC: American Soc for Microbiology; 1993:414(a1616).
10. Meffre C, Girard R, Hajjar J, Fabry J. Is peripheral venous catheter colonisation related to the antiseptic used for disinfection of the insertion site? Povidone-iodine vs. alcoholic chlorhexidine: a multicenter randomised prospective
study [Abstract]. Catheter Study Group. Hygienes. 1995;9:45.
11. Mimoz O, Pieroni L, Lawrence C, Edouard A, Costa Y, Samii K, et al.
Prospective, randomized trial of two antiseptic solutions for prevention of central
venous or arterial catheter colonization and infection in intensive care unit patients. Crit Care Med. 1996;24:1818-23. [PMID: 8917031]
12. Legras A, Cattier B, Dequin PF, Boulain T, Perrotin D. Etude prospective
randomisee pour la prevention des infections liees aux catheters: chlorhexidine
alcoolique contre polyvidone iodee. Reanimation et Urgences. 1997;6:5-11.
13. LeBlanc A, Cobett S. IV site infection: a prospective, randomized clinical trial
comparing the efficacy of three methods of skin antisepsis. Canadian Intravenous
Nurses Association Journal. 1999;15:48-50.
14. Humar A, Ostromecki A, Direnfeld J, Marshall JC, Lazar N, Houston PC,
et al. Prospective randomized trial of 10% povidone-iodine versus 0.5% tincture
of chlorhexidine as cutaneous antisepsis for prevention of central venous catheter
infection. Clin Infect Dis. 2000;31:1001-7. [PMID: 11049783]
15. Brun-Buisson C, Abrouk F, Legrand P, Huet Y, Larabi S, Rapin M. Diagnosis of central venous catheter-related sepsis. Critical level of quantitative tip
cultures. Arch Intern Med. 1987;147:873-7. [PMID: 3555377]
16. Maki DG, Weise CE, Sarafin HW. A semiquantitative culture method for
identifying intravenous-catheter-related infection. N Engl J Med. 1977;296:
1305-9. [PMID: 323710]
17. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials.
1986;7:177-88. [PMID: 3802833]
18. Petitti DB. Meta-Analysis, Decision Analysis, and Cost-Effectiveness Analysis. 2nd ed. New York: Oxford Univ Pr; 2000.
19. Light RJ, Pillemer DB. Summing Up: The Science of Reviewing Research.
Cambridge, MA: Harvard Univ Pr; 1984.
20. Donner A, Klar N. Design and Analysis of Cluster Randomization Trials in
Health Research. London: Arnold; 2000.
21. Mallaret MR, Duc DL, Manquat G, Berthieux M. Chlorhexidine or povidone iodine for intravascular catheter maintenance: a bibliographical review. Medecine et Maladies Infectieuses. 1997;27:827-32.
22. Pearson ML. Guideline for prevention of intravascular device-related infecwww.annals.org
Antiseptic for Catheter-Site Care: A Meta-Analysis
tions. Part I. Intravascular device-related infections: an overview. The Hospital
Infection Control Practices Advisory Committee. Am J Infect Control. 1996;24:
262-77. [PMID: 8870910]
23. Saint S, Veenstra DL, Lipsky BA. The clinical and economic consequences
of nosocomial central venous catheter-related infection: are antimicrobial catheters useful? Infect Control Hosp Epidemiol. 2000;21:375-80. [PMID:
10879567]
24. Veenstra DL, Saint S, Sullivan SD. Cost-effectiveness of antiseptic-impregnated central venous catheters for the prevention of catheter-related bloodstream
infection. JAMA. 1999;282:554-60. [PMID: 10450717]
25. Peacock SJ, Bowler IC, Crook DW. Positive predictive value of blood cultures growing coagulase-negative staphylococci [Letter]. Lancet. 1995;346:191-2.
[PMID: 7603263]
26. Gottardi W. Iodine and iodine compounds. In: Block SS, ed. Disinfection,
Sterilization, and Preservation. 4th ed. Philadelphia: Lea & Febiger; 1991:15166.
27. Zamora JL, Price MF, Chuang P, Gentry LO. Inhibition of povidoneiodine’s bactericidal activity by common organic substances: an experimental
study. Surgery. 1985;98:25-9. [PMID: 4012604]
28. Lowbury EJ, Lilly HA. The effect of blood on disinfection of surgeons’
hands. Br J Surg. 1974;61:19-21. [PMID: 4204415]
29. Larson E, Bobo L. Effective hand degerming in the presence of blood.
J Emerg Med. 1992;10:7-11. [PMID: 1629595]
30. Denton WG. Chlorhexidine. In: Block SS, ed. Disinfection, Sterilization,
and Preservation. 4th ed. Philadelphia: Lea & Febiger; 1991:274-89.
31. Ayliffe GA. Surgical scrub and skin disinfection. Infect Control. 1984;5:23-7.
[PMID: 6358087]
www.annals.org
Article
32. Smylie HG, Logie JR, Smith G. From Phisohex to Hibiscrub. Br Med J.
1973;4:586-9. [PMID: 4586059]
33. Shelton DM. A comparison of the effects of two antiseptic agents on Staphylococcus epidermidis colony forming units at the peritoneal dialysis catheter exit
site. Adv Perit Dial. 1991;7:120-4. [PMID: 1680406]
34. Okano M, Nomura M, Hata S, Okada N, Sato K, Kitano Y, et al. Anaphylactic symptoms due to chlorhexidine gluconate. Arch Dermatol. 1989;125:
50-2. [PMID: 2910207]
35. Ebo DG, Stevens WJ, Bridts CH, Matthieu L. Contact allergic dermatitis
and life-threatening anaphylaxis to chlorhexidine. J Allergy Clin Immunol. 1998;
101:128-9. [PMID: 9449513]
36. Torricelli R, Wuthrich B. Life-threatening anaphylactic shock due to skin
¨
application of chlorhexidine [Letter]. Clin Exp Allergy. 1996;26:112. [PMID:
8789551]
37. Yong D, Parker FC, Foran SM. Severe allergic reactions and intra-urethral
chlorhexidine gluconate. Med J Aust. 1995;162:257-8. [PMID: 7891607]
38. Snellman E, Rantanen T. Severe anaphylaxis after a chlorhexidine bath. J Am
Acad Dermatol. 1999;40:771-2. [PMID: 10321611]
39. Russell AD, Day MJ. Antibacterial activity of chlorhexidine. J Hosp Infect.
1993;25:229-38. [PMID: 7907620]
40. Darouiche RO, Raad II, Heard SO, Thornby JI, Wenker OC, Gabrielli A,
et al. A comparison of two antimicrobial-impregnated central venous catheters.
Catheter Study Group. N Engl J Med. 1999;340:1-8. [PMID: 9878638]
41. Veenstra DL, Saint S, Saha S, Lumley T, Sullivan SD. Efficacy of antisepticimpregnated central venous catheters in preventing catheter-related bloodstream
infection: a meta-analysis. JAMA. 1999;281:261-7. [PMID: 9918482]
4 June 2002 Annals of Internal Medicine Volume 136 • Number 11 801
Coments go here:
- Log in to post comments