Utilization of Biocompatible Adhesive/Sealant Materials for Securing Surgical Devices
Utilization of Biocompatible Adhesive/Sealant Materials for Securing Surgical Devices
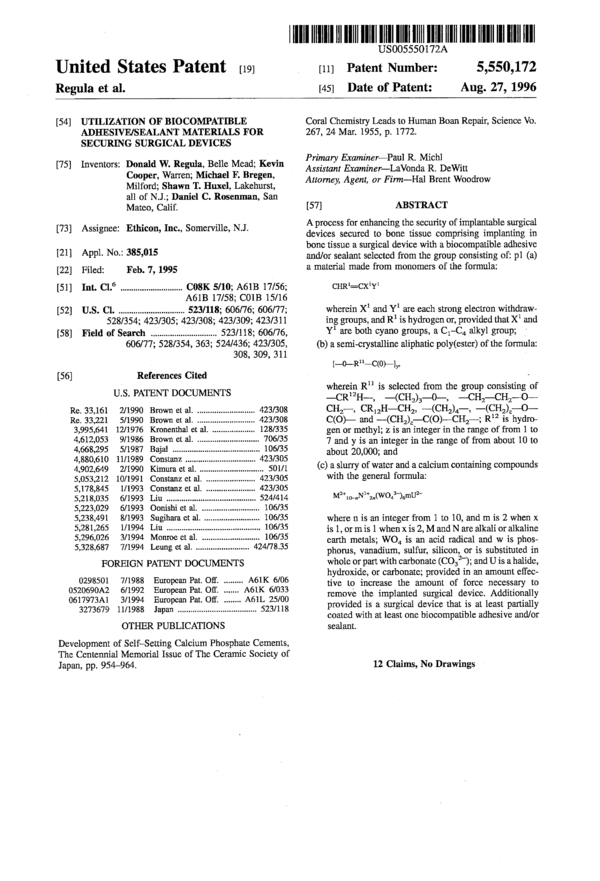
US5550172
Company:
Folder:
Year:
Abstract:
A process for enhancing the security of implantable surgical devices secured to bone tissue comprising implanting in bone tissue a surgical device with a biocompatible adhesive and/or sealant selected from the group consisting of: p1 (a) a material made from monomers of the formula:
Type of document:
Language:
United States Patent [191
Regula et al.
ll|I||||||||l|Ill|||||||l||||||||||||Illll||l||llllll||||||||||||||||l|l||l
US005550172A
Patent Number:
5,550,172
Aug. 27, 1996
[111
[45] Date of Patent:
[54] UTILIZATION OF BIOCOMPATIBLE
ADI-IESIVE/SEALANT MATERIALS FOR
SECURING SURGICAL DEVICES
[75] Inventors: Donald W. Regula, Belle Mead; Kevin
Cooper, Warren; Michael F. Bregen,
Milford; Shawn T. Huxel, Lakehurst,
all of N.J.; Daniel C. Rosenman, San
Mateo, Calif.
[73] Assignee: Ethicon, Inc., Somerville, N.J.
[21] Appl. No.: 385,015
[22] Filed: Feb. 7, 1995
[51] Int. C1.° ........................... .. C08K 5/10; A61B 17/56;
A6lB 17/58; C01B 15/16
[52] U.S. Cl. ............................. .. 523/118; 606/76; 606/77;
528/354; 423/305; 423/308; 423/309; 423/311
[58] Field of Search ............................. .. 523/118; 606/76,
606/77; 528/354, 363; 524/436; 423/305,
308, 309, 311
[56] References Cited
U.S. PATENT DOCUMENTS
Re. 33,161 2/1990 Brown et al. 423/308
Re. 33,221 5/1990 Brown et al. 423/308
3,995,641 12/1976 Kronenthal et al. . .. 128/335
4,612,053 9/1986 Brown et al. . . . . . . . . . . . . .. 706/35
4,668,295 5/1987 Bajal . . . . . . . . . . . . . . . . . . . .. 106/35
4,880,610 11/1989 Constanz ....... .. 423/305
4,902,649 2/1990 Kimura et al. .. ...... .. 501/1
5,053,212 10/1991 Constanz et al. 423/305
5,178,845 1/1993 Constanz et al. 423/305
5,218,035 6/1993 Liu ................ .. 524/414
5,223,029 6/1993 Oonishiet al. . .... .. 106/35
5,238,491 8/1993 Sugihaxa et al. .... .. 106/35
5,281,265 1/1994 Liu . . . . . . . . . . . . . . . . . . . . . . .. 106/35
5,296,026 3/1994 Monroe et al. . ........ .. 106/35
5,328,687 7/1994 Leung et al. ....................... .. 424/78.35
FOREIGN PATENT DOCUMENTS
0298501 7/1988 European Pat. Off. ....... .. A61K 6/06
0520690A2 6/1992 European Pat. Off. ..... .. A6lK 6/033
0617973Al 3/1994 European Pat. Off. ...... .. A6lL 25/00
3273679 11/1988 Japan ................................... .. 523/118
OTHER PUBLICATIONS
Development of Self—Setting Calcium Phosphate Cements,
The Centennial Memorial Issue of The Ceramic Society of
Japan, pp. 954-964.
Coral Chemistry Leads to Human Boan Repair, Science V0.
267, 24 Mar. 1955, p. 1772.
Primary Examiner—Pau1 R. Michl
Assistant Examiner—LaV0nda R. DeWitt
Attomey, Agent, or Firm—Hal Brent Woodrow
[57] ABSTRACT
A process for enhancing the security of implantable surgical
devices secured to bone tissue comprising implanting in
bone tissue a surgical device with a biocompatible adhesive
and/or sealant selected from the group consisting of: pl (a)
a material made from monomers of the formula:
Cl-IR‘=CX‘lY‘
wherein X‘ and Y1 are each strong electron withdraw-
ing groups, and R‘ is hydrogen or, provided that X‘ and
Y1 are both cyano groups, a C1-C4 alkyl group; _
(b) a serni-crystalline aliphatic poly(ester) of the formula:
1—o—R“—c(o>—1,.
wherein R” is selected from the group consisting of
—CR‘2H——, —(CH2)3—0—, ——CH2—CH2-—O——
CH2——, CR12H—CH2, ——(CH2)4—, —(CH2)z—-O-—
C(O)— and ——(CH2)z—C(O)—CH2——; R” is hydro-
gen or methyl; z is an integer in the range of from 1 to
7 and y is an integer in the range of from about 10 to
about 20,000; and
(c) a slurry of water and a calcium containing compounds
with the general formula:
Ml+1o—nN1+2n(wO43_)amU27
where n is an integer from 1 to 10, and m is 2 when x
is 1, or m is 1 when x is 2, M and N are alkali or alkaline
earth metals; W04 is an acid radical and w is phos-
phorus, vanadium, sulfur, silicon, or is substituted in
whole or part with carbonate (CO32'); and U is a halide,
hydroxide, or carbonate; provided in an amount effec-
tive to increase the amount of force necessary to
remove the implanted surgical device. Additionally
provided is a surgical device that is at least partially
coated with at least one biocompatible adhesive and/or
sealant.
12 Claims, No Drawings
5,550,172
1
UTILIZATION OF BIOCOMPATIBLE
ADHESIVE/SEALANT MATERIALS FOR
SECURING SURGICAL DEVICES
FIELD OF THE INVENTION
This invention relates to securing surgical repair devices
to tissue, more specifically this invention relates to securing
surgical devices such as screws, plates, bone pins and
anchors to bone tissue.
BACKGROUND OF THE INVENTION
In orthopedic surgery it is often necessary to reattach
cartilage and ligaments to skeletal bones with surgical pins,
screws or anchors. For example, metallic suture anchors are
currently used to facilitate cartilage or ligament reattach-
ment. In these procedures a hole is drilled into the skeletal
bone. A suture anchor, attached to a suture, is then inserted
into the hole in a manner that allows the anchor to engage
the sides of the hole and be held in place. The suture is then
used to secure the torn cartilage or ligament to the bone.
However, sometimes during or after the healing process
these anchors fail to remain in place and must be removed
to avoid harm to the patient.
Recently, absorbable suture anchors have been proposed
as a replacement for metallic suture anchors. The perceived
advantage of an absorbable anchor over the metallic anchor
is that after the healing process for the cartilage or ligament
is complete the anchor will be absorbed by the patient’s
body and disappear. However, most bioabsorbable materials
are not strong enough to dig into bone tissue. Therefore,
bioabsorbable bone anchors tend to have less resistance to
being pulled out of the location in which it is secured.
Thus, it would be a significant contribution to the art to
provide a method to enhance the secure placement of
implantable surgical devices in patients. Additionally, it
would be advantageous if a method could be developed to
enhance the resistance to removal of bioabsorbable surgical
implantable devices.
SUMMARY OF THE INVENTION
We have discovered a process for enhancing the security
of implantable surgical devices secured to bone tissue com-
prising implanting a surgical device with a biocompatible
adhesive and/or sealant provided in an amount effective to
increase the security of the implanted surgical device.
In another embodiment of the present invention we have
also provided an implantable surgical device comprising an
implantable surgical device coated with a biocompatible
adhesive or sealant.
DETAILED DESCRIPTION OF THE
INVENTION
The present invention provides a process for using a
surgical device that improves the security and placement of
the surgical device in a mammalian body. Also described is
an implantable surgical device which has been coated with
a biocompatible adhesive or sealant in an amount sufficient
to facilitate the placement of the surgical device in the
desired location in a patient. Suitable surgical devices which
may benefit from having an adhesive or sealant coating
include but are not limited to surgical screws, pins, plates,
anchors, rods, clamps, clips, staples, rivets, hooks, buttons,
snaps and the like.
20
25
30
35
45
50
55
60
65
l
2
These surgical devices may be made from a biocompat-
ible material using conventional fabrication methods. The
clips can be composed of various biocompatible metals, e.g.
titanium and tantalum, and polymeric materials. Preferred
bioabsorbable polymeric materials include homopolymers
and copolymers of epsilon-caprolactone, glycolide, lactide,
para-dioxanone, and trimethylene carbonate. Preferred non-
absorbable polymers include nylons, polyesters and
polypropylene. All these materials have been demonstrated
to be biologically acceptable when used as sutures or other
implantable "medical devices.
The preferred means for fabricating surgical devices from
polymeric materials is to inject a suitable polymer melt into
an appropriately designed mold at process conditions con-
ventionally employed for such polymer systems. After the
polymer melt cools, the molded polymer shaped in the mold
to meet the design criteria of the device can be readily
released from the mold.
One class of suitable biocompatible adhesives or sealants
that can be used in the practice of the present invention
include materials made from monomers of the formula:
CI-lR‘=CX‘Y‘ (1)
wherein X1 and Y‘ are each strong electron withdrawing
groups, and R1 is hydrogen or, provided that X’ and Y1 are
both cyano groups, a C1-C4 alkyl group. Examples of
monomers within the scope of formula (I) include ot-cy-
anoacrylates, vinylidene cyanides, C1-C4 alkyl homologues
of vinylidene cyanides, dialkyl methylene malonates, acy-
lacrylonitriles, vinyl sulfinates, and vinyl sulfonates of the
formula CH2=CX2Y2 wherein X2 is SOZRZ or —SO3R2
and Y2 is —CN, COOR2, COCH3, —SO2R2 or —SO3R2
and R2 is hydrogen or an alkyl group.
Preferred monomers of formula (I) for use in this inven-
tion are alpha-cyanoacrylates. These monomers are known
in the art and have the formula
CN (11)
CI-IR3=C
COOR4
wherein R3 is hydrogen and R4 is a hydrocarbon or substi-
tuted hydrocarbon group; a group having the formula
—R5—O—R°—O—R7, wherein R5 is a 1,2-alkylene group
having 2-4 carbon atoms, R6 is an alkylene group having
2-4 carbon atoms, and R7 is an alkyl group having 1-6
carbon atoms; or a group having the formula:
—R8—c—o—R9 (111)
I I
0
wherein R8 is
as
—CH—,
.—CH;—-,
or —C(CH3)2—and R9 is an organic radical.
Examples of suitable hydrocarbon and substituted hydro-
carbon groups include straight chain or branched chain alkyl
groups having l—l6 carbon atoms; straight chain or
branched chain C1—C,6 alkyl groups substituted with one or
more biologically compatible substituents such as an acy-
loxy group, an alkoxy group, an aryloxy group, a haloalkyl
group, a halogen atom, a dialkylamino group, an alkylary-
lamino group, or a cyano group; straight chain or branched
chain alkenyl groups having 2 to 16 carbon atoms; straight
chain or branched chain alkynyl groups having 2 to 12
5,550,172
3
carbon atoms; cycloalkyl groups; arylalkyl groups; alkylaryl
groups and aryl groups
In the cyanoacrylate monomer of formula (II), R4 is
preferably an alkyl group having 1-10 carbon atoms or a
group having the formula —AOR1°, wherein A is a divalent
straight or branched chain alkylene or oxyalkylene radical
having 2-8 carbon atoms, and R” is a straight or branched
alkyl radical having 1-8 carbon atoms. Examples of groups
represented by the formula —AOR‘° include 1-methoxy-2-
propyl, 2-butoxy ethyl, isopropoxy-ethyl, and 2-ethoxy
ethyl.
The most preferred alpha-cyanoacrylate monomers used
in this invention are methyl alpha-cyanoacrylate, butyl
alpha-cyanoacrylate, octyl alpha-cyanoacrylate, 1-methoxy—
2-propyl cyanoacrylate, 2-butoxy ethyl cyanoacrylate, and
isopropoxy-ethyl cyanoacrylate.
The alpha—cyanoacrylates of formula (11) wherein R4 is a
hydrocarbon or substituted hydrocarbon group can be pre-
pared according to methods known in the art. Reference is
made, for example, to U.S. Pat. Nos. 2,721,858 and 3,254,
111, each of which is hereby incorporated by reference
herein. For example, the alpha-cyanoacrylates can be pre-
pared by reacting an alkyl cyanoacetate with formaldehyde
in a non-aqueous organic solvent and in the presence of a
basic catalyst, followed by pyrolysis of the anhydrous inter-
mediate polymer in the presence of a polymerization inhibi-
tor. The alpha-cyanoacrylate monomers prepared with low
moisture content and essentially free of impurities are pre-
ferred for biomedical use.
The alpha-cyanoacrylates of formula (II) wherein R4 is a
group having the formula R5——O—R“—O—R7 can be pre-
pared according to the method disclosed in U.S. Pat. No.
4,364,876 (Kimura et al.), which is hereby incorporated by
reference herein. In the Kimura et al. method, the alpha-
cyanoacrylates are prepared by producing a cyanoacetate by
esterifying cyanoacetic acid with an alcohol or by transes-
terifying an alkyl cyanoacetate and an alcohol; condensing
the cyanoacetate and formaldehyde or para-forrnaldehyde in
the presence of a catalyst at a molar ratio of 0.5—1.5:1,
preferably 0.8-1.211, to obtain a condensate; depolymeriz-
ing the condensation reaction mixture either directly or after
removal of the condensation catalyst to yield crude
cyanoacrylate; and distilling the crude cyanoacrylate to form
a high purity cyanoacrylate.
The alpha-cyanoacrylates of formula (11) wherein R4 is a
group having the formula
_..R8.._fi_0_R9
O
can be prepared according to the procedure described in
U.S. Pat. No. 3,995,641 (Kronenthal et al.), which is
hereby incorporated by reference herein. In the Kronenthal
et al. method, such alpha-cyanoacrylate monomers are pre-
pared by reacting an alkyl ester of an alpha-cyanoacrylic
acid with a cyclic 1,3-diene to form a Diels-Alder adduct
which is then subjected to alkaline hydrolysis followed by
acidification to form the corresponding alpha-cyanoacrylic
acid adduct. The alpha-cyanoacrylic acid adduct is prefer-
ably esterified by an alkyl bromoacetate to yield the corre-
sponding carbalkoxymethyl alpha-cyanoacrylate adduct.
Altematively, the alpha-cyanoacrylic acid adduct may be
converted to the alpha-cyanoacrylyl halide adduct by reac-
tion with thionyl chloride. The alpha-cyanoacrylyl halide
adduct is then reacted with an alkyl hydroxyacetate or a
methyl substituted alkyl hydroxyacetate to yield the corre-
sponding carbalkoxymethyl alpha-cyanoacrylate adduct or
20
25
30
35
40
45
50
55
60
65
4
carbalkoxy alkyl alpha-cyanoacrylate adduct, respectively.
The cyclic 1,3-diene blocking group is finally removed and
the carbalkoxy methyl alpha-cyanoacrylate adduct or the
carbalkoxy alkyl alpha-cyanoacrylate adduct is converted
into the corresponding carbalkoxy alkyl alpha-cyanoacrylate
by heating the adduct in the presence of a slight deficit of
malcic anhydride.
Another type of biocompatible adhesives or sealant that
may be used in the practice of the present invention are
copolymers of formula (I) or one monomer of formula (I)
and a monomer of the formula:
Cl-lZ=CX‘Y‘ (IV)
wherein X‘ and Y1 are as described for formula (I) and Z is
——CH=CH2. Examples of monomers of formula (IV)
include cyanopentadienoates and alpha-cyanoacrylates of
the formula:
CN
/
Cl-IZ=C
(V)
COOR4
wherein Z is —CH=CH2 and R4 is as defined above. The
monomers of formula (IV) wherein R4 is an alkyl group of
1-10 carbon atoms, i.e., the 2-cyanopenta-2,4-dienoic acid
esters, can be prepared by reacting an appropriate 2-cy-
anoacetate with acrolein in the presence of a catalyst such as
zinc chloride. This method of preparing 2-cyanopenta-2,4,
4-dienoic acid esters is disclosed, for example, in U.S. Pat.
No. 3,554,990, which is hereby incorporated by reference
herein.
Optionally, a biocompatibilizing agent may be added to
the cyanoacrylate adhesive such as are disclosed in U.S. Pat.
No. 5,328,687, hereby incorporated by reference.
Suitable bioabsorbable sealants include semi-crystalline
aliphatic ester homopolymers, and copolymers made from
polymers of the formula:
[—0—R“—C(0)-ly. (V1)
wherein R“ is selected from the group consisting of
——CR‘2H—, —(CH2)3——O—, —CH2—CH2——-O—CH2——,
CR‘2H-—CH2, —(CH2)4—, —(CH2)z—O—C(O)—-and
—(CH2)z——C(O)——CH2—; R12 is hydrogen or methyl; z is
an integer in the range of from 1 to 7; and y is an integer in
the range of from about 10 to about 20,000.
Many nontoxic bioabsorbable aliphatic ester polymers
that are semi-crystalline solids at room temperature, may be
used in the present invention. The polymers of this invention
are generally characterized as being solids at body tempera-
ture (37° C.) and preferably will be melt at temperatures of
less than 60° C. Suitable bioabsorbable polymers include
solid poly(e-caprolactone), poly(p-dioxanone), or poly(tri-
methylene carbonate) homopolymers and copolymers of
e-caprolactone and trimethylene carbonate. Copolymers of
e-caprolactone should be composed of from about 100 mole
percent to about 70 mole percent and preferably from 95
mole percent to 85 mole percent of e-caprolactone repeating
units with the remainder of the polymer being a plurality of
second lactone repeating units. The second lactone repeating
units will be selected from the group consisting of glycolide
repeating units, lactide repeating units, 1,4-dioxanone
repeating units, 1,4-dioxepan—2-one repeating units, 1,5-
dioxepan-2-one repeating units, trimethylene carbonate
repeating units, and combinations thereof. Preferred are
copolymers of e-caprolactone that are semicrystalline solids
at body temperature. The solid polymers of trimethylene
5,550,172
5
carbonate should be composed of from in the range of from
about 1 to about 20 mole percent or from about 100 to about
80 mole percent of trimethylene carbonate with the remain-
der of the copolymer being composed of a plurality of '
lactone repeating units selected from the group consisting of
glycolide repeating units, lactide repeating units, p-diox-
anone repeating units, e-caprolactone repeating units, and
combinations thereof.
It is preferred for the trimethylene carbonate copolymers
to have crystalline regions formed by the second lactone
repeating units wherein the crystalline regions provide at
least 5 percent crystallinity to the final copolymer. The solid
polymers may be linear, branched, or star branched; block
copolymers or terpolymers; segmented block copolymers or
terpolymers. These polymers will also be purified to sub-
stantially remove unreacted monomers which may cause an
inflammatory reaction in tissue. The most preferred poly-
mers for use as the adhesive/sealant are semicrystalline
polymers selected from the group consisting of poly(e-
caprolactone), poly(e-caprolactone-co-trimethylene carbon-
ate), poly(e-caprolactone-co-lactide), po1y(e-caprolactone-
co-p-dioxanone), and poly(e-caprolactone-co-glycolide).
The mole percent of e-caprolactone repeating units in these
polymers should be in the range of from 100 to about 80
mole percent and preferably in the range of from 95 to 85
mole percent. Most preferably these polymers will be sta-
tistically random copolymers.
The polymers used as the adhesive/sealant should have an
inherent viscosity as determined in a 0.1 g/dL solution of
hexafluoroisopropanol (HFIP) at 25° C. ranging from about
0.1 dL/g to about 2.0 dIJg, preferably from about 0.15 dL/g
to about 1.5 dL/g, and most preferably from 0.2 dL/g to 1.0
dL/g. A polymer with an inherent viscosity below 0.1 dL/g
may fail to crystallize at room temperature, and a polymer
with an inherent viscosity above 2.0 dL/g may make the
polymer have too high of a melting point.
The aliphatic poly(ester)s-are generally prepared by a ring
opening polymerization of the desired proportions of one or
more lactone monomers in the presence of an organometal-
lic catalyst and an initiator at elevated temperatures. The
organometallic catalyst is preferably a tin-based catalyst,
e.g. stannous octoate, and is present in the monomer mixture
at a molar ratio of 10 monomer to catalyst ranging from
about 15,000/1 to about 80,000/ 1. The initiator is typically
an alkanol (such as 1-dodecanol), a polyol (such as 1,2-
propanediol, 1,3-propanediol, diethylene glycol, or glycerol,
poly(ethylene glycol)s, poly(propylene glycol)s and poly-
(ethylene-co-propylene glycol)s), a hydroxyacid, or an
amine, and is present in the monomer mixture at a molar
ratio of monomer to initiator ranging from about 100/1 to
about 5000/1. The polymerization is typically carried out at
a temperature range from about 80° to about 220° C.,
preferably 160° to 190° C., until the desired molecular
weight and viscosity are achieved.
The aliphatic polyesters described above will be solids at
room temperature but may be heated to provide a putty like
or liquid material that may be applied as a sealant to support
surgical devices or to secure a surgical device. In one
embodiment of the present invention, the aliphatic polyester
would be heated to its melting point and applied to the
desired location before it resolidified. In this embodiment, if
a bone pin were inserted in a hole drilled in bone tissue,
melted polyester would be poured into the hole before or
after the pin was inserted to help secure the bone pin in the
bone tissue. Alternatively, the aliphatic polyester could be
heated until it softens and then used as a putty and placed at
the desired location and act as a filler.
20
25
30
35
40
45
50
55
60
65
6
Other suitable bioabsorbable sealants include calcium
containing compounds with the general formula:
M2+1o—nN1+2n(wO43_)6mUx-
where n is an integer from 1 to 10, and m is 2 when X is 1,
or m is 1 when x is 2, M and N are alkali or alkaline earth
metals, preferably calcium, magnesium, sodium, zinc, and
potassium. W04 is an acid radical, where W is preferably
phosphorus, vanadium, sulfur or silicon, or is substituted in
whole or part with carbonate (CO32‘). U is an anion,
preferably halide, hydroxide, or carbonate.
Most preferred are calcium containing sealants selected
from the group consisting of mono-, di-, octa-, on-tri-, B-tri-,
or tetra-calcium phosphate, hydroxyapatite, fluorapatite, cal-
cium sulfate, calcium fluoride and mixtures thereof.
The calcium containing sealants can also contain a bio-
active glass comprising metal oxides such as calcium oxide,
silicon dioxide, sodium oxide, phosphorus pentoxide, and
mixtures thereof, and the like. The calcium containing
sealants will preferably have a particle size of about 10
microns to about 1000 microns, and more preferably about
100 microns to about 500 microns.
The calcium containing sealants will generally be applied
in an aqueous slurry. The amount of calcium containing
material in the slurry will generally be in the range from
about 10 weight percent to about 90 weight percent. The
slurry will preferably be retained in place at the desired
location until it solidifies or develops a putty like consis-
tency.
The adhesive and/or sealant may be applied to at least one
surface of the medical device that is to be contacted with the
bone tissue or applied to the site where the surgical device
is to be secured. For example, when a bone pin or anchor is
placed in a hole drilled in bone tissue the pin or anchor
surfaces that will contact the bone tissue will be coated with
adhesive and placed in intimate contact with the bone tissue.
The adhesive will then adhere to the device and the bone and
enhance the security of the pin or anchor in the hole.
Alternatively, the adhesive may be applied to the site where
the surgical device is to be secured and the surgical device
applied thereafter in an appropriate time so that the adhesive
or sealant can set. If a sealant is used the sealant may serve
as a filling and support agent for the medical device. For
example, when using a bone plate with multiple openings for
fasteners (such as screws), the sealant would be applied to
the surface to contact the bone to provide a putty like base
on which to mount the bone plate on to simplify installation
of the bone plate.
Those skilled in the art will readily be able to determine
the appropriate amount of adhesive and/or sealant to apply
in a given surgical application. Similarly, the amount of an
adhesive and/or sealant to be applied to a surgical device
before implantation will be a discretionary matter depending
on the operation and the specific circumstances of the
operation.
The adhesives and/or sealants of the present invention
will generally be applied in a liquid form. The adhesive
and/or sealant will generally be applied through a small
diameter delivery device such as a syringe, with or without
mechanical assistance, a caulking gun, a soft-sided tube, and
the like.
The following nonlimiting examples are provided to
illustrate the practice of the present invention.
EXAMPLE 1
Synthesis of the Anthracene Adduct of Dimethyl Meth-
ylidene Malonate. 178.0 grams (1.00 mol) of powdered
5,550,172
7
anthracene, 60.0 grams (2.00 mol) of powdered paraforrn-
aldehyde, 132.0 grams (1.00 mol) of dimethyl malonate,
10.0 grams (50 mmol) of cupric acetate monohydrate, 225
mL of glacial acetic acid, and 450 mL of xylene were added
to a two liter, three necked, round bottom flask. In the
exhaust hood, the flask was immersed into an oil bath and
secured with a clamp. A mechanical stirrer, a stainless steel
thermocouple connected to a therrnowatch which controlled
the immersion heater, and a water cooled distillation appa-
ratus were then installed. The still was connected to a dry
nitrogen gas line via a Firestone valve. The contents of the
reaction flask were heated to 100° C. for 18 hours; then, the
pot temperature was raised until the azeotropic mixture of
acetic acid, water, and xylene started to distill out. The oil
bath temperature ranged 125° C. to 145° C. during the
distillation. The still head temperature varied from 95° 1 C.
to 110° C. When most of the solvents were removed, the
resulting suspension was allowed to cool down to room
temperature. The residue was dissolved in chloroform, and
in portions, transferred into a separatory funnel, washed with
an equal volume of saturated ammonium chloride solution,
washed with saturated sodium chloride solution, dried over
anhydrous magnesium sulfate, and suction filtered. The
filtrate was transferred into a round bottom flask and the
chloroform removed by evaporation. The crude product
[305 grams; 95% yield, but impure] was then recrystallized
from xylene [1 grarn/2 mL] using activated charcoal at —5°
C. 228 grams of recrystallized adduct were collected [75%
recovery; 71% yield overall, although the material is still
contaminated with small amounts of anthracene]. The mate-
rial was recrystallized again to produce about 188 grams of
doubly recrystallized adduct [82% recovery; 58% yield
overall; still contained some anthracene]. The material was
recrystallized again yielding 158 grams of triply recrystal-
lized material [84% recovery; 49% overall yield]. The
crystals were isolated by suction filtration, washed with
methanol, and vacuumed dried at 50° C. after each recrys-
tallization.
EXAMPLE 2
Synthesis of Dimethyl Methylidene Malonate (DMMM).
500 grams of mineral oil, 120.0 grams (373 mmol) of the
anthracene adduct of dimethyl methylidene malonate, 64.9
grams (375 mmol) of N-phenylmaleimide, and 050 grams
(3.5 mmol) of phosphorous pentoxide were added to a
silanized, flame dried, one liter round bottom flask contain-
ing a magnetic stirring bar. This mixture was degassed on a
vacuum manifold overnight. Then, a silanized distillation
head and fraction cutter were installed, and the flask
immersed in an oil bath already set at 225° C. under a
nitrogen atmosphere. After fifteen minutes, a yellow solution
was obtained. One hour later, the oil bath was removed and
the contents of the flask were allowed to cool down to 50°
C. High vacuum was then applied to the reaction system. A
pressure of around 450 microns was typical in the beginning
of the distillation, and the pressure fell to around 300
microns by the end of the distillation. Once the system
stabilized at low pressure, the dimethyl methylidene mal-
onate distilled over between 50° C. and 55° C. [the oil bath
temperature ranged from 50° C. to around 70° C.]. 31.0
grams of dimethyl methylidene malonate were collected in
the middle fraction [58% yield;>99 mole % pure by NMR
spectroscopy].
EXAMPLE 3
synthesis of Poly[e-caprolactone] (PCL). In the glove
box, l°uL (40 umol) of a 0.33M stannous octoate solution in
10
20
25
30
35
45
50
55
60
65
8
toluene, 2.3 mL (24 mmol) of distilled diethylene glycol,
and 205.3 grams (1.8 mol) of distilled e-caprolactone were
transferred into a silanized, flame dried, 500 mL, round
bottom flask equipped with a stainless steel mechanical
stirrer and a nitrogen gas blanket. The reaction flask was
immersed in an oil bath already set at 75° C. After fifteen
minutes, a clear solution was obtained and then the oil bath
temperature was raised to 190° C. for 19 hours. The stirrer
blade was removed, and the polymer melt was allowed to
cool down to room temperature in an inert atmosphere. After
about two hours, the polymer started to crystallize and
became opaque. The polymer was isolated by wrapping the
flask in aluminum foil, freezing the flask in liquid nitrogen,
and removing the broken glass. Then, the frozen polymer
was ground on a Wiley mill and sieved through a screen.
35.2 grams of a fine powder were saved; 161.8 grams of the
coarse grounds were vacuum dried at 40° C. for 12 hours.
160.9 grams of devolatized PCL were collected. The PCL
was vacuum dried again under the same conditions without
any weight loss. The inherent viscosity was measured in
chloroform at 25° C. and found to be 0.3 dL/g [c=0.10 g/dL].
The number average molecular weight was 9,000 glmol and
the weight average molecular weight was 16,000 glmol as
determined by gel permeation chromatography in HFIP
using PMMA standards. The monomer conversion was 97.6
mole percent as determined by 300 MHZ ‘H NMR spectrum
in HFAD/CGDE; 2.4 mole percent unreacted monomer was
also detected. The polymer melted between 60° C. and 65°
C. using a Fisher-Johns apparatus.
In the glove box, 25 grams of PCL and 0.25 grams of
sucrose [a nucleating agent] were added to a silanized, flame
dried, 100 mL, round bottom flask equipped with a stainless
steel mechanical stirrer and a nitrogen gas blanket. The
reaction flask was immersed in an oil bath set at 125°C.
After the PCL had melted, the mixture was blended for one
hour and then allowed to cool down to room temperature
under .an inert atmosphere. The polymer was isolated by
wrapping the flask in aluminum foil, freezing the flask in
liquid nitrogen, and removing the broken glass. The frozen
polymer was crushed and vacuum dried at room temperature
overnight and then stored under nitrogen gas until used in
the bone pin study described below.
EXAMPLE 4
Bone Pin Pullout Force Measurements. Materials and
Methods: Rabbit femurs were cleaned and frozen. They
were defrosted before testing and allowed to warm up to 37°
C. A hole was drilled in the femoral condyle with a 2.7 mm
drill bit. Bone pins made of poly[glycolie acid] having a
nominal diameter of 2.8 mm were roughened with sand
paper to improve adhesion and were inserted into the
femoral condyle with no adhesive, with Vetbond (n-butyl
cyanoacrylate), dimethyl methylene malonate (DMMM)
from Example 2 and with low molecular weight poly[e-
caprolactone] (PCL) from Example 3. The cure time was
one minute for the Vetbond and DMMM and thirty minutes
for the low molecular weight PCL. Mechanical testing was
conducted on an Instron model 1122 tensile tester at a cross
head speed of 0.5 inches per minute. The femur was held in
the bottom fixture, and the bone pin was pulled out by the
upper fixture. The force was measured and the maximum
force recorded.
Results: The pullout force data are summarized in Table
1. These data clearly show that the average pullout force
increased significantly when an adhesive was used; the
increase in pullout strength varied from 4 to 11 times that of
5,550,172
9
the force needed to remove the bone pin without any glue
being applied.
TABLE 1
Pullout Strengths
Pullout Strengths (kg)
Bone Pin
Test Only Vetbond DMMM PCL
1 ‘ 0.661 6.95 3.43 2.3
2 0.765 8.35 7.41 2.94
3 — 9.82 6.79 2.19
4 — 5.66 2.27 3.41
Average 0.71 7.70 4.98 2.71
We claim:
1. A process for enhancing the security of implantable
surgical devices secured to bone tissue consisting essentially
of securing a surgical device with a biocompatible adhesive
and/or sealant selected from the group consisting of:
(a) a bioabsorbable semi-crystalline aliphatic poly(ester)
of the formula:
[-0-—R“-C(0)-ly,
wherein R” is selected from the group consisting of
—CR‘2H—, —(CH2)3—O—, —CH2—CH2 —
CH2—, CR‘2H—CH2, —(CH2)4—, —(CH2)z—O—
C(O)— and —(CH2)Z—C(O)—CH2—; R12 is hydro-
gen or methyl; z is an integer in the range of from 1 to
7 and y is an integer in the range of from about 10 to
about 20,000; and
(b) a slurry of water and a calcium containing compound
with the general formula:
M2+t.HN‘+2...mU*-
where n is an integer form 1 to 10, and m is 2 when x
is l, or In is 1 when x is 2, M and N are alkali or alkaline
earth metals; W04 is an acid radical and W is phos—
phorus, vanadium, sulfur, silicon, or is substituted in
whole or part with carbonate (CO32_); and U is a
halide hydroxide, or carbonate; provided in an amount
eifective to increase the amount of force necessary to
remove the implanted surgical device.
2. The process of claim 1 wherein the sealant and/or
adhesive is applied to the site where the implantable surgical
device is to be secured. -
3. The process of claim 1 wherein the surgical device is
selected from the group consisting of screws, pins, plates,
anchors, rods, clamps, clips, staples, rivets, hooks, buttons
and snaps.
4. The process of claim 1 wherein the surgical device is
made of a bioabsorbable polymeric material.
5. The process of claim 1 wherein the adhesive and/or
sealant is a bioabsorbable serni-crystalline aliphatic poly-
(ester) homopolymer selected from the group consisting of
poly(e-caprolactone), poly(p-dioxanone), and poly(trimeth—
ylene carbonate).
6. A process for enhancing the security of implantable
surgical devices secured to bone tissue comprising securing
a surgical device to bone with a bioabsorbable semi-crys-
talline aliphatic poly(ester) copolymer composed of from
about 100 mole percent to about 70 mole percent of e-ca-
prolactone repeating units with the remainder of the polymer
being a plurality of second lactone repeating unit selected
10
20
25
30
35
45
50
55
60
65
10
from the group consisting of glycolide repeating units,
lactide repeating units, 1,4-dioxanone repeating units, 1,4-
dioxepan-2-one repeating units, 1,5-dioxepan-2-one repeat-
ing units, trimethylene carbonate repeating units, and com-
binations thereof provided in an amount effective to increase
the amount of force necessary to remove the implanted
surgical device.
7. The process of claim 1 wherein the adhesive and/or
sealant is applied to the implantable surgical device and the
surgical device is then secured to the bone tissue.
8. An implantable surgical device consisting essential of
an implantable surgical device that is at least partially coated
with a biocompatible adhesive and/or sealant selected from
the group consisting of:
(a) a bioabsorbable semi-crystalline aliphatic poly(ester)
of the formula:
[—0—R”—C(0)—]y,
wherein R“ is selected from the group consisting of
—CR‘_2H——, —(CH2)3-—O—, —CH2——CH2—O—
CH2—, CR‘2H—CH2, —(CH2)4—, —(CH2)Z
—O—C(O)— and —(CH2)z—C(0)—CH2—; R12 is
hydrogen or methyl; 2 is an integer in the range of from
1 to 7 and y is an integer in the range of from about 10
to about 20,000; and
(b) a slurry of water and a calcium containing compound
with the general formula:
M2+ro_,.N”;..(W043“)smU"- '
where n is an integer from 1 to 10, and m is 2 when x
is 1, or m is 1 when x is 2, M and N are alkali or alkaline
earth metals; W04 is an acid radical and W is phos-
phorus, vanadium, sulfur, silicon, or is substituted in
whole or part with carbonate (CO32“); and U is a halide,
hydroxide, or carbonate; provided in an amount effec-
tive to increase the amount of force necessary to
remove the implanted surgical device.
9. The surgical devices of claim 8 wherein the surgical
device is selected from the group consisting of screws, pins,
plates, anchors, rods, clamps, clips, staples, rivets, hooks,
buttons and snaps.
10. The surgical device of claim 8 wherein the surgical
device is made of a bioabsorbable polymeric material.
11. The surgical device of claim 8 wherein the adhesive
and/orsealant that at least partially coats the surgical device
is a bioabsorbable semi-crystalline aliphatic poly(ester)
homopolymer selected from the group consisting of poly(e-
caprolactone), poly(p-dioxanone), and poly(trimethylene
carbonate).
12. An implantable surgical device comprising an
implantable surgical device that is at least partially coated
with a bioabsorbable semi-crystalline aliphatic poly(ester)
copolymer composed of from about 100 mole percent to
about 70 mole percent of e-caprolactone repeating units with
the remainder of the polymer being a plurality of second
lactone repeating units selected from the group consisting of
glycolide repeating units, lactide repeating units, 1,4-diox-
anone repeating units, 1,4-dioxepan-2-one repeating units,
1,5-dioxepan-2-one repeating units, trimethylene carbonate
repeating units, and combinations thereof provided in an
amount efl"'ective to increase the amount of force necessary
to remove the implanted surgical device.
* * * * *
Coments go here:
- Log in to post comments